Blood Levels of Long-Chain n–3 Fatty Acids and the Risk of Sudden Death
Christine M. Albert, M.D., M.P.H., Hannia
Campos, Ph.D., Meir J. Stampfer,
M.D., Dr.P.H., Paul M. Ridker,
M.D., M.P.H., JoAnn E. Manson, M.D., Dr.P.H., Walter C. Willett, M.D., Dr.P.H.,
and Jing Ma, M.D., Ph.D.
ABSTRACT
Background Experimental data suggest that long-chain n–3 polyunsaturated fatty acids found in fish have antiarrhythmic properties, and a randomized trial suggested that dietary supplements of n–3 fatty acids may reduce the risk of sudden death among survivors of myocardial infarction. Whether long-chain n–3 fatty acids are also associated with the risk of sudden death in those without a history of cardiovascular disease is unknown.
Methods We conducted a prospective, nested case–control analysis among apparently healthy men who were followed for up to 17 years in the Physicians' Health Study. The fatty-acid composition of previously collected blood was analyzed by gas–liquid chromatography for 94 men in whom sudden death occurred as the first manifestation of cardiovascular disease and for 184 controls matched with them for age and smoking status.
Results Base-line blood levels of long-chain n–3 fatty acids were inversely related to the risk of sudden death both before adjustment for potential confounders (P for trend = 0.004) and after such adjustment (P for trend = 0.007). As compared with men whose blood levels of long-chain n–3 fatty acids were in the lowest quartile, the relative risk of sudden death was significantly lower among men with levels in the third quartile (adjusted relative risk, 0.28; 95 percent confidence interval, 0.09 to 0.87) and the fourth quartile (adjusted relative risk, 0.19; 95 percent confidence interval, 0.05 to 0.71).
Conclusions The n–3 fatty acids found in fish are strongly associated with a reduced risk of sudden death among men without evidence of prior cardiovascular disease.
We previously reported that fish consumption was associated with a reduced risk of sudden death from cardiac causes, but not a reduced risk of myocardial infarction, in the Physicians' Health Study.1 It is hypothesized that the long-chain n–3 polyunsaturated fatty acids found in fish, primarily eicosapentaenoic acid and docosahexaenoic acid, may be responsible for this association. Experimental data from studies in animals and at the cellular level suggest that these n–3 fatty acids have antiarrhythmic properties,2,3 and a recent randomized trial testing supplements of these n–3 fatty acids in survivors of myocardial infarction found a statistically significant 45 percent reduction in the risk of sudden death, with no effect on nonfatal myocardial infarction.4 However, prospective data on blood levels of long-chain n–3 fatty acids and sudden death from cardiac causes are sparse, and there have been no randomized trials of the effects of long-chain n–3 fatty acids in the diet or as supplements among persons without a history of cardiovascular disease, who represent over half of all cases of sudden death from cardiac causes.5
To address the hypothesis that the long-chain n–3 fatty acids found in fish are associated with a reduced risk of sudden death from cardiac causes in those without known cardiovascular disease, we performed a prospective, nested case–control analysis of the fatty-acid composition of whole blood in men without a confirmed history of cardiovascular disease who were participants in the Physicians' Health Study.
Methods
Study Population and Collection of Whole-Blood Samples
The methods of the Physicians' Health Study have been described in detail elsewhere.6,7 Briefly, 22,071 male physicians, who were 40 to 84 years old in 1982 and had no history of myocardial infarction, stroke, transient ischemic attacks, or cancer, were assigned at random according to a two-by-two factorial design to receive aspirin, beta carotene, both active drugs, or both placebos. Informed consent was obtained from all subjects, and the research protocol was approved by the institutional review board at Brigham and Women's Hospital in Boston. At base line, the physicians completed questions on their health status and risk factors for cardiovascular disease. Dietary intake of fish was ascertained at 12 months with an abbreviated, semiquantitative food-frequency questionnaire,8 as described previously.1 Information on cardiovascular events was updated every six months for the first year and annually thereafter with follow-up questionnaires.
Before randomization, which occurred between August 1982 and December 1984, potential participants were asked to provide base-line blood samples, which were collected in EDTA and processed for long-term storage at –80°C. Of the randomized study participants, 14,916 (68 percent) provided base-line blood samples. More than 70 percent of these specimens were received between September and November 1982.
Confirmation of End Points and Selection of Controls
The end point of sudden death from cardiac causes was ascertained by a two-step process. First, deaths from any cause were generally reported by postal authorities or next of kin, and an end-point review committee confirmed deaths from cardiovascular causes by examining medical records obtained from hospitals and attending physicians. A participant's next of kin was interviewed about the circumstances of the death if they were not adequately documented in the medical record.
Second, to ascertain the specific end point of sudden death from cardiac causes, two cardiologists who were unaware of the subject's exposure status reviewed medical records and reports from the next of kin of all deaths from cardiovascular causes (excluding strokes). In this second review, sudden death from cardiac causes was defined as death within one hour after the onset of symptoms or a witnessed cardiac arrest or abrupt collapse that occurred within one hour after the onset of symptoms and that resulted in death. For all these deaths, no probable noncardiac cause was suggested by the history or autopsy. To increase specificity for death from cardiac arrhythmia, we excluded any death for which there was evidence of collapse of the circulation (hypotension, exacerbation of congestive heart failure, or altered mental status) before the disappearance of the pulse.9 Unwitnessed deaths with no information on timing but with an autopsy report consistent with death from cardiac arrhythmia (i.e., acute coronary thrombosis or severe coronary artery disease without myocardial necrosis or other pathological findings to explain death) were considered possible sudden deaths from cardiac causes. Analyses were performed both including and excluding these deaths, with similar results.
Over the 17 years of study follow-up, 201 sudden deaths from cardiac causes were documented; for 119 of these, an adequate base-line blood sample was available for analysis. Ninety-four of these subjects had been free of confirmed cardiovascular disease before death. Each of these subjects was matched with two control subjects, who had also provided an adequate base-line blood sample and who were alive and remained free of confirmed cardiovascular disease at the time of case ascertainment. A diagnosis of confirmed cardiovascular disease required a report of angina with a positive stress-test result or coronary angiography documenting clinically significant coronary artery disease, myocardial infarction confirmed according to World Health Organization criteria, or stroke confirmed by a typical neurologic deficit lasting longer than 24 hours. Using a risk-set sampling method, we randomly selected controls from among study participants who met the matching criteria for age (within one year), smoking status (formerly, currently, or never), and length of time since randomization (in six-month intervals). For four case subjects, only one adequate control could be found.
Laboratory Analysis
Whole blood collected and stored at base line was thawed. Although there
are no data on their long-term storage in blood, long-chain n–3
fatty acids have been documented to have high reliability coefficients
(0.64 to 0.66) and minimal oxidation in serum samples stored at
–80°C for up to 12 years.10 The fatty acids from
whole blood were extracted11,12 and quantitated by
gas–liquid chromatography on a fused silica capillary cis–trans column (SP2560, Supelco,
Statistical Analysis
For base-line risk factors, means or proportions were calculated for men who died suddenly (case subjects) and controls. The significance of associations was tested with the chi-square statistic for categorical variables and with Student's t-test for continuous variables. Associations between base-line risk factors and levels of long-chain n–3 fatty acids, expressed as percentages of total fatty acids, were tested with Student's t-test. The Spearman rank-correlation coefficient was used to test the association between base-line levels of long-chain n–3 fatty acids and fish consumption, measured at 12 months.
Means (expressed as percentage of total fatty acids) for each fatty-acid peak were calculated for case and control subjects, and the significance of differences was tested by Student's t-test for those that were normally distributed and the Wilcoxon rank-sum test for those that were not normally distributed. To estimate the relative risk of sudden death according to the blood level of long-chain n–3 fatty acids, we first categorized each subject according to quartiles determined by the distribution of fatty acid levels in the controls. We then performed logistic-regression analysis, conditioned on the matching variables of age and smoking. Adjusted estimates of risk were obtained with multivariate models that also controlled for body-mass index; presence or absence of a history of diabetes, hypertension, or hyperlipidemia; presence or absence of a parental history of premature myocardial infarction; alcohol intake; frequency of physical activity; and random assignment to aspirin and beta carotene or placebo. After the quartile analysis suggested a linear relation, tests for trend were performed by entering a continuous variable in the conditional-regression model.
In secondary analyses, to assess for confounding by other fatty acids, each fatty-acid group (saturated, monounsaturated, n–6 polyunsaturated, and trans unsaturated fatty acids) was entered separately according to quartile into the multivariate model, and the change in the parameter estimate for the continuous value of long-chain n–3 fatty acid was observed. If a change of more than 15 percent was noted, the fatty acid remained in this multivariate model. All P values were two-tailed, and all confidence levels were computed at the 95 percent level.
Results
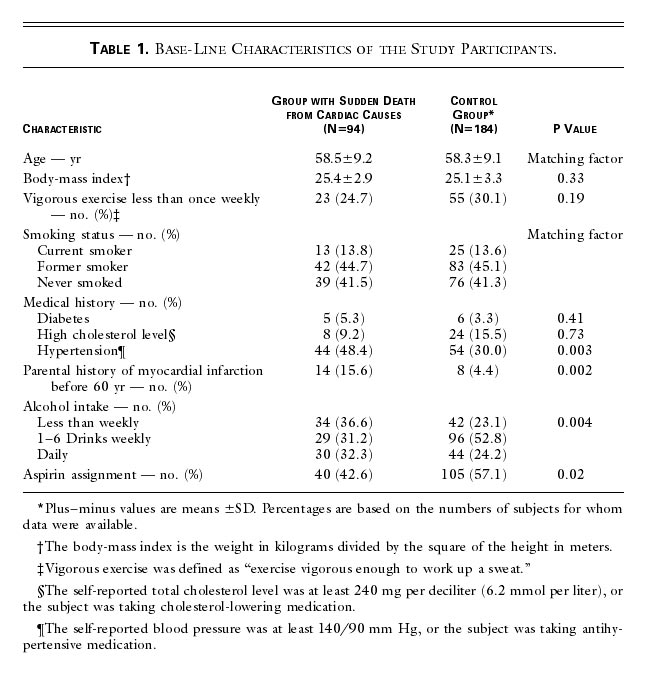
Table 1 shows the base-line characteristics of the 94 subjects in
whom sudden death was the first manifestation of cardiovascular disease
and the 184 matched controls. The mean time from study enrollment to
sudden death was 8.7 years (range, 0.7 to 16.9). In this sample, the
men who died suddenly were significantly more likely to have a
history of hypertension, significantly more likely to have a
parental history of early coronary artery disease (i.e., before 60
years of age), and significantly less likely to have been randomly
assigned to receive aspirin. The relation with alcohol intake was
U-shaped: men who died suddenly were more likely to drink less than
once a week or daily, and less likely to drink one to six drinks per
week. Of the risk factors listed in Table 1, significantly lower
levels of long-chain n–3 fatty acids were found among current
smokers than among former smokers or those who had never smoked
(mean [±SD], 4.47±1.31 vs. 5.20±1.30 percent of total fatty acids;
P=0.002). In addition, the base-line blood level of long-chain n–3
fatty acids was significantly correlated with fish intake at 12
months (R2=0.24, P=0.001) (data not shown).
|
|
The base-line blood levels of each major fatty acid among men who
died suddenly and controls are shown in Table 2. The mean level of
total long-chain n–3 fatty acids was significantly lower among the
men who died suddenly than among the controls (4.82±1.31 vs.
5.24±1.32 percent of total fatty acids, P=0.01). In contrast, the
levels of the other fatty acids, including the short-chain n–3
polyunsaturated fatty acid (![]() -linolenic acid), saturated fatty acids, monounsaturated
fatty acids, n–6 polyunsaturated fatty acids, and trans unsaturated
fatty acids, did not differ significantly between men who died suddenly
and control subjects.
-linolenic acid), saturated fatty acids, monounsaturated
fatty acids, n–6 polyunsaturated fatty acids, and trans unsaturated
fatty acids, did not differ significantly between men who died suddenly
and control subjects.
|
|
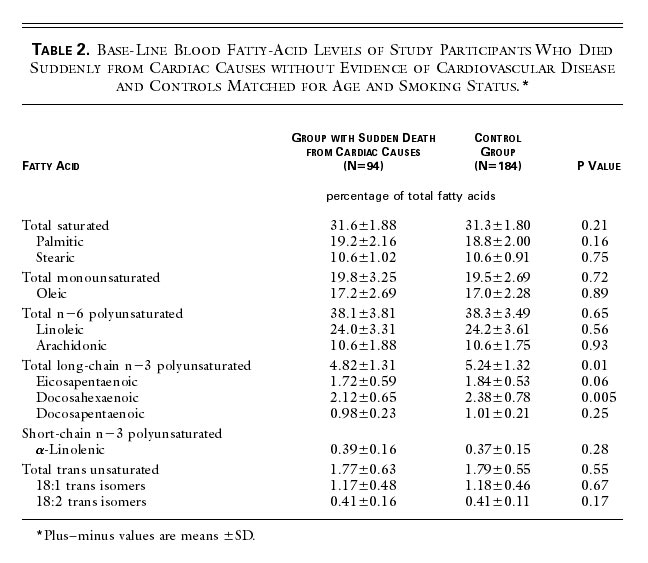
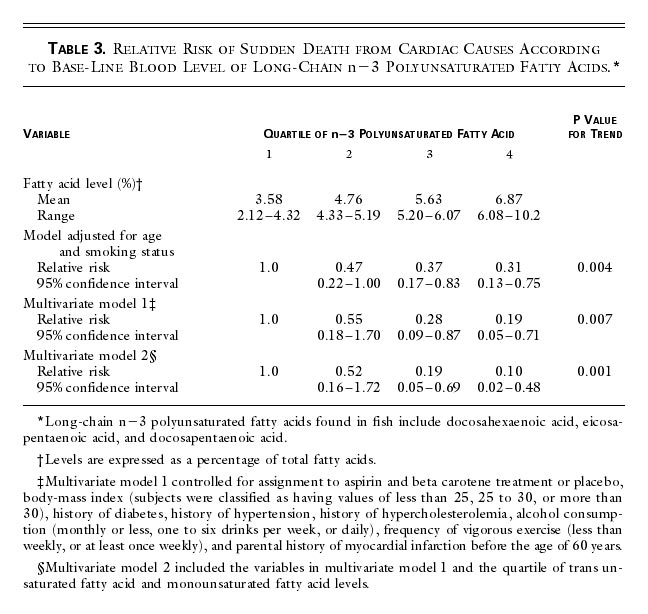
Table 3 shows the relation of base-line blood levels of long-chain n–3
fatty acids to the risk of sudden death. The level of long-chain n–3
fatty acids was significantly inversely related to the risk of
sudden death in both the analysis adjusted for age and smoking
status (P for trend = 0.004) and the multivariate analysis (P for trend
= 0.007). As compared with the men with levels of long-chain n–3
fatty acids in the lowest quartile (mean, 3.58 percent of total
fatty acids), those with levels in the highest quartile (mean, 6.87
percent) had a relative risk of sudden death of 0.19 (95 percent
confidence interval, 0.05 to 0.71) after known confounders were
controlled for (multivariate model 1). These results were not
materially affected when 15 possible sudden deaths were excluded
from the analysis (relative risk for highest vs. lowest quartile,
0.14; 95 percent confidence interval, 0.03 to 0.75; P for trend =
0.01).
|
|
Since the level of long-chain n–3 fatty acids was significantly associated
with levels of other fatty acids (inversely with saturated, trans
unsaturated, and monounsaturated fatty acids and directly with n–6
polyunsaturated fatty acids), each fatty-acid group was entered in
the multivariate model to evaluate the independent association of
long-chain n–3 fatty acids with the risk of sudden death. Adjustment
for saturated and n–6 polyunsaturated fatty acids did not
appreciably alter the association between long-chain n–3
polyunsaturated fatty acids and the risk of sudden death. Adjustment
for monounsaturated and trans unsaturated
fatty acids resulted in a further strengthening of the relation (Table
3, multivariate model 2). With this adjustment, the relative risk of
sudden death among men with levels of long-chain n–3 fatty acids in
the highest quartile as compared with the lowest quartile was 0.10
(95 percent confidence interval, 0.02 to 0.48; P for trend = 0.001).
Discussion
In this prospective, nested case–control study of healthy male physicians without evidence of cardiovascular disease at enrollment, the base-line blood level of long-chain n–3 fatty acids was inversely associated with the subsequent risk of sudden death, even after known confounders had been controlled for. The association was linear, with a statistically significant inverse trend across quartiles of levels of long-chain n–3 fatty acids. As compared with men with levels of long-chain n–3 fatty acids in the lowest quartile, those with levels in the highest quartile had an 81 percent lower risk of sudden death. This relation persisted when blood levels of other fatty-acid groups were controlled for in the model. Therefore, the association did not appear to depend on compensatory changes in the levels of other fatty acids.
These prospective findings are remarkably similar to those reported in a population-based case–control study involving 82 cases of primary cardiac arrest.13 That study found a strong inverse association between red-cell n–3 fatty-acid composition at the time of the arrest and the risk of primary cardiac arrest among subjects with no history of clinically recognized cardiac disease. Taken together, these data support the hypothesis that long-chain n–3 fatty acids are responsible for the observed inverse association between fish consumption and sudden death.1,13 There was no evidence of a threshold effect for blood levels of long-chain n–3 fatty acids, although a threshold effect was previously reported for fish intake in this cohort.1
Because the present study did not examine other cardiovascular end points or death from other causes, we cannot present direct data on the selectivity of the association between long-chain n–3 fatty acids and sudden death. However, previous studies of this cohort found no association between plasma levels of long-chain n–3 fatty acids14 or fish intake1 and the risk of myocardial infarction. In addition, a selective beneficial effect on the risk of sudden death was found in a randomized trial.4 In that trial, men with a history of myocardial infarction who were assigned to a fish-oil supplement had a statistically significant 45 percent reduction in the risk of sudden death, which translated into an overall significant reduction in total mortality. However, there was no reduction in the risk of nonfatal cardiovascular events or in other causes of mortality.
The apparent beneficial effect on the risk of sudden death from cardiac causes in observational studies and randomized trials could be due in part to the antiarrhythmic effects of n–3 fatty acids, as reported from experimental models.3,15,16 Plausible mechanisms for these antiarrhythmic effects include modulation of sodium, potassium, and L-type calcium channels2,17,18; inhibition of thromboxane production19,20; and beneficial effects on heart-rate variability.21,22 Other indirect effects of long-chain n–3 fatty acids include lowering of the nonesterified fatty-acid concentration in plasma and cell membranes. Nonesterified fatty acids have multiple proarrhythmic properties and have recently been associated with an increased risk of sudden death, but not of fatal myocardial infarction, among men enrolled in the Paris Prospective Study I.23
The limitations of these data merit consideration. First, our analyses
are based on a single base-line measurement and therefore may not
accurately reflect levels of long-chain n–3 fatty acids over long
periods. Furthermore, although the coefficients of variation were
low, misclassification due to laboratory error cannot be ruled out.
It is important to note, however, that neither of these sources of
variability can account for the strong inverse association we
observed between long-chain n–3 fatty acid levels and sudden death,
since any random misclassification would bias results toward the
null hypothesis. The use of a single base-line measurement does,
however, limit our ability to assess accurately the relation between
the shorter-chain n–3 fatty acid, ![]() -linolenic acid, and sudden death, since this
fatty acid is largely metabolized,24 and if it is
stored, it is elongated to docosahexaenoic
acid. Therefore, blood levels of
-linolenic acid, and sudden death, since this
fatty acid is largely metabolized,24 and if it is
stored, it is elongated to docosahexaenoic
acid. Therefore, blood levels of ![]() -linolenic acid would be more dependent on what foods were
eaten recently and less likely to reflect average dietary intake.
-linolenic acid would be more dependent on what foods were
eaten recently and less likely to reflect average dietary intake.
The use of whole blood is a possible limitation, because it combines two different pools of long-chain n–3 fatty acids, the plasma and the stored red-cell pools. Alternatively, this composite measure may be viewed as a strength, since these pools have different half-lives and provide complementary information. Finally, as with any observational study, the inverse association between blood levels of long-chain n–3 fatty acids and sudden death could be due, at least in part, to residual confounding by other dietary and lifestyle factors. However, control for major known confounders and other fatty-acid groups had little effect on the estimates of relative risk.
In summary, taken together with previous data from observational studies
and randomized trials, these prospective data suggest that the
long-chain n–3 fatty acids found in fish may reduce the risk of
sudden death from cardiac causes, even among men without a history
of cardiovascular disease. Because more than 50 percent of all
sudden deaths from cardiac causes occur in people with no history of
cardiac disease,5
preventive efforts must address this segment of the population to
have a substantial effect on the overall incidence of sudden death
from cardiac causes. If the observed association is causal,
increasing the intake of n–3 fatty acids by eating more fish or by
taking supplements is an intervention that could be applied to this
segment of the population at low cost and little risk.
Supported by grants from the National Institutes of Health (CA-34944, CA-40360, HL-26490, and HL-34595) and by a Mentored Clinical Scientist Development Award (1-K08-HL-03783) from the National Heart, Lung, and Blood Institute (to Dr. Albert).
Source Information
From the Division of Preventive Medicine (C.M.A., P.M.R., J.E.M.), the Channing Laboratory (M.J.S., J.E.M., W.C.W., J.M.), and the Division of Cardiovascular Medicine (P.M.R.), Department of Medicine, Brigham and Women's Hospital; the Cardiovascular Division, Department of Medicine, Massachusetts General Hospital (C.M.A.); and the Departments of Nutrition (H.C., M.J.S., W.C.W.) and Epidemiology (M.J.S., J.E.M., W.C.W.), Harvard School of Public Health — all in Boston.
Address reprint requests to Dr. Albert at the
Division of Preventive Medicine, Brigham and Women's Hospital,
References
- Albert
CM, Hennekens CH, O'Donnell CJ, et al. Fish
consumption and risk of sudden cardiac death. JAMA 1998;279:23-28.
[Abstract/Full Text]
- Kang JX, Leaf A. Antiarrhythmic effects of polyunsaturated fatty acids:
recent studies. Circulation 1996;94:1774-1780.
[Full Text]
- Billman
GE, Kang JX, Leaf A. Prevention of sudden cardiac death by dietary pure
 -3 polyunsaturated fatty
acids in dogs. Circulation 1999;99:2452-2457.
-3 polyunsaturated fatty
acids in dogs. Circulation 1999;99:2452-2457.[Abstract/Full Text]
- GISSI-Prevenzione Investigators (Gruppo Italiano per lo Studio della Sopravvivenza nell'Infarto Miocardico). Dietary supplementation with n-3 polyunsaturated fatty acids and vitamin E after myocardial infarction: results of the GISSI-Prevenzione trial. Lancet 1999;354:447-455. [Erratum, Lancet 2000;357:642.][CrossRef][ISI][Medline]
- Kannel WB, Schatzkin A. Sudden death: lessons from subsets in population studies. J Am Coll Cardiol 1985;5:Suppl B:141B-149B.[Medline]
- The Steering Committee of the Physicians' Health Study Research Group. Preliminary report: findings from the aspirin component of the ongoing Physicians' Health Study. N Engl J Med 1988;318:262-264.[ISI][Medline]
- The Steering Committee of the Physicians' Health Study Research Group. Final report on the aspirin component of the ongoing Physicians' Health Study. N Engl J Med 1989;321:129-135.[Abstract]
- Willett WC, Sampson L, Stampfer MJ, et al. Reproducibility and validity of a semiquantitative food frequency questionnaire. Am J Epidemiol 1985;122:51-65.[Abstract]
- Hinkle KE, Thaler HT. Clinical classification of cardiac deaths. Circulation 1982;65:457-464.[Abstract]
- Zeleniuch-Jacquotte A, Chajes V, Van Kappel AL, Riboli E, Toniolo P. Reliability of fatty acid composition in human serum phospholipids. Eur J Clin Nutr 2000;54:367-372.[CrossRef][ISI][Medline]
- Zock P, Gerristen J, Katan M. Partial conservation of the sn-2 position of dietary triglycerides in fasting plasma lipids in humans. Eur J Clin Invest 1996;26:141-150.[ISI][Medline]
- Zock PL, Mensink RP, Harryvan J, de Vries JH, Katan MB. Fatty acids in serum cholesteryl esters as quantitative biomarkers of dietary intake in humans. Am J Epidemiol 1997;145:1114-1122.[Abstract]
- Siscovick DS, Raghunathan TE, King I, et al. Dietary intake and cell membrane levels of long-chain n-3 polyunsaturated fatty acids and the risk of primary cardiac arrest. JAMA 1995;274:1363-1367.[Abstract]
- Guallar E, Hennekens CH, Sacks FM, Willett WC, Stampfer MJ. A prospective study of plasma fish oil levels and incidence of myocardial infarction in U.S. male physicians. J Am Coll Cardiol 1995;25:387-394.[CrossRef][ISI][Medline]
- Billman
GE, Hallaq H, Leaf A. Prevention of
ischemia-induced ventricular fibrillation by
 3
fatty acids. Proc Natl Acad
Sci U S A 1994;91:4427-4430.[Abstract]
3
fatty acids. Proc Natl Acad
Sci U S A 1994;91:4427-4430.[Abstract]
- McLennan PL, Bridle TM, Abeywardena MY, Charnock JS. Dietary lipid modulation of ventricular fibrillation threshold in the marmoset monkey. Am Heart J 1992;123:1555-1561.[ISI][Medline]
- Xiao YF, Gomez AM, Morgan
JP, Lederer WJ, Leaf A. Suppression of
voltage-gated L-type Ca2+ currents by polyunsaturated fatty
acids in adult and neonatal rat ventricular myocytes.
Proc Natl Acad Sci U S A 1997;94:4182-4187.
[Abstract/Full Text]
- Xiao Y-F, Wright SN, Wang
GK, Morgan JP, Leaf A. Fatty acids suppress voltage-gated Na+
currents in HEK293t cells transfected with the
alpha-subunit of the human cardiac Na+ channel. Proc Natl Acad Sci U S A 1998;95:2680-2685.
[Abstract/Full Text]
- Nair SSD, Leitch JW, Falconer J, Garg
ML. Prevention of cardiac arrhythmia by dietary (n-3) polyunsaturated
fatty acids and their mechanism of action. J Nutr
1997;127:383-393.
[Abstract/Full Text]
- Li Y, Kang JX, Leaf A. Differential effects of various eicosanoids on the production or prevention of arrhythmias in cultured neonatal rat cardiac myocytes. Prostaglandins 1997;54:511-530.[CrossRef][Medline]
- Christensen JH, Korup E, Aaroe J, et al. Fish consumption, n-3 fatty acids in cell membranes, and heart rate variability in survivors of myocardial infarction with left ventricular dysfunction. Am J Cardiol 1997;79:1670-1673.[CrossRef][ISI][Medline]
- Christensen JH, Skou HA, Fog L, et al. Marine n-3 fatty acids, wine
intake, and heart rate variability in patients referred for coronary
angiography. Circulation 2001;103:651-657.
[Abstract/Full Text]
- Jouven
X, Charles MA, Desnos M, Ducimetiere
P. Circulating nonesterified fatty acid level as
a predictive risk factor for sudden death in the population. Circulation
2001;104:756-761.
[Abstract/Full Text]
- Cunnane
SC, Anderson MJ. The majority of dietary linoleate
in growing rats is
 -oxidized or stored in
visceral fat. Nutrition 1997;127:146-152.
-oxidized or stored in
visceral fat. Nutrition 1997;127:146-152.
|
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||
n–3 Fatty Acids
and the Risk of Sudden Death
Henriques J. P.S., Zijlstra
F., Siguel E., Hrdy D. B., Knecht T. P., Albert C. M., Stampfer
M. J., Ma J., Rosenberg I. H.
N Engl J Med 2002; 347:531-533,
This article has been cited by other articles:
- Holguin,
F., Tellez-Rojo, M. M., Lazo,
M., Mannino, D., Schwartz, J., Hernandez, M., Romieu, I. (2005). Cardiac Autonomic Changes
Associated With Fish Oil vs Soy Oil
Supplementation in the Elderly. Chest 127: 1102-1107
[Abstract] [Full Text] - Arita,
M., Bianchini, F., Aliberti,
J., Sher, A., Chiang, N., Hong, S., Yang, R., Petasis, N. A., Serhan, C.
N. (2005). Stereochemical assignment, antiinflammatory properties, and receptor for the
omega-3 lipid mediator resolvin E1. J. Exp.
Med. 201: 713-722
[Abstract] [Full Text] - Arnold, S. M., Lynn, T. V., Verbrugge, L. A., Middaugh,
J. P. (2005). Human Biomonitoring to Optimize
Fish Consumption Advice: Reducing Uncertainty When Evaluating Benefits and
Risks. Am J Public Health 95: 393-397
[Abstract] [Full Text] - Oh, R. (2005). Practical
Applications of Fish Oil ({Omega}-3 Fatty Acids) in Primary Care. J Am
Board Fam Pract
18: 28-36
[Abstract] [Full Text] - Geelen,
A., Brouwer, I. A, Schouten,
E. G, Maan, A. C, Katan,
M. B, Zock, P. L (2005). Effects of n-3 fatty
acids from fish on premature ventricular complexes and heart rate in
humans. Am. J. Clin. Nutr.
81: 416-420
[Abstract] [Full Text] - Mozaffarian,
D., Ascherio, A., Hu,
F. B., Stampfer, M. J., Willett, W. C., Siscovick, D. S., Rimm, E.
B. (2005). Interplay Between Different Polyunsaturated Fatty Acids and
Risk of Coronary Heart Disease in Men. Circulation 111: 157-164
[Abstract] [Full Text] - Roberts, C. K., Barnard, R.
J. (2005). Effects of exercise and diet on chronic disease. J. Appl. Physiol. 98: 3-30
[Abstract] [Full Text] - Oliver, M. F. (2002). Sudden
unexpected cardiac death. Eur Heart
Journal 23: 1797-1798
[Full Text] - Giltay,
E. J, Gooren, L. J., Toorians,
A. W., Katan, M. B, Zock,
P. L (2004). Docosahexaenoic acid concentrations
are higher in women than in men because of estrogenic effects. Am. J. Clin. Nutr. 80:
1167-1174
[Abstract] [Full Text] - Folsom, A. R., Demissie, Z. (2004). Fish Intake, Marine Omega-3 Fatty
Acids, and Mortality in a Cohort of Postmenopausal Women. Am. J. Epidemiol. 160: 1005-1010
[Abstract] [Full Text] - Harris, W. S., Sands, S. A.,
Windsor, S. L., Ali, H. A., Stevens, T. L., Magalski,
A., Porter, C. B., Borkon, A. M. (2004). Omega-3
Fatty Acids in Cardiac Biopsies From Heart Transplantation Patients:
Correlation With Erythrocytes and Response to Supplementation. Circulation
110: 1645-1649
[Abstract] [Full Text] - Benatti,
P., Peluso, G., Nicolai,
R., Calvani, M. (2004). Polyunsaturated Fatty
Acids: Biochemical, Nutritional and Epigenetic Properties. J Am Coll Nutr 23: 281-302
[Abstract] [Full Text] - Erkkila,
A. T, Lichtenstein, A. H, Mozaffarian, D.,
Herrington, D. M (2004). Fish intake is associated with a reduced
progression of coronary artery atherosclerosis in postmenopausal women
with coronary artery disease. Am. J. Clin. Nutr. 80: 626-632
[Abstract] [Full Text] - Dangour,
A. D., Sibson, V. L., Fletcher, A. E. (2004). Hormones and Supplements: Do
They Work?: Micronutrient Supplementation in Later Life: Limited Evidence
for Benefit. J Gerontol A Biol Sci Med Sci 59: B659-B673
[Abstract] [Full Text] - Mozaffarian,
D., Psaty, B. M., Rimm,
E. B., Lemaitre, R. N., Burke, G. L., Lyles, M.
F., Lefkowitz, D., Siscovick,
D. S. (2004). Fish Intake and Risk of Incident Atrial
Fibrillation. Circulation 110: 368-373
[Abstract] [Full Text] - Paoletti,
R., Gotto, A. M. Jr, Hajjar, D. P. (2004). Inflammation in Atherosclerosis
and Implications for Therapy. Circulation 109: III-20-III-26
[Abstract] [Full Text] - Surette,
M. E., Edens, M., Chilton, F. H., Tramposch, K. M. (2004). Dietary Echium
Oil Increases Plasma and Neutrophil Long-Chain
(n-3) Fatty Acids and Lowers Serum Triacylglycerols
in Hypertriglyceridemic Humans. J. Nutr. 134: 1406-1411
[Abstract] [Full Text] - Theobald,
H. E, Chowienczyk, P. J, Whittall,
R., Humphries, S. E, Sanders, T. A. (2004). LDL cholesterol-raising effect
of low-dose docosahexaenoic acid in middle-aged
men and women. Am. J. Clin. Nutr. 79: 558-563
[Abstract] [Full Text] - Din, J. N, Newby, D. E, Flapan, A. D (2004). Omega 3 fatty acids and
cardiovascular disease--fishing for a natural treatment. BMJ 328:
30-35
[Full Text] - Dwyer, J. H., Allayee, H., Dwyer, K. M., Fan, J., Wu, H., Mar, R., Lusis, A. J., Mehrabian, M.
(2004). Arachidonate 5-Lipoxygenase Promoter
Genotype, Dietary Arachidonic Acid, and
Atherosclerosis. N Engl J Med 350:
29-37
[Abstract] [Full Text] - Harris, W. S., O'Keefe, J.
H. Jr, Grundy, S. M. (2003). Preventive Use of
N-3 Fatty Acids * Response. Circulation 108: e139-139
[Full Text] - Dallongeville,
J., Yarnell, J., Ducimetiere,
P., Arveiler, D., Ferrieres,
J., Montaye, M., Luc, G., Evans, A., Bingham,
A., Hass, B., Ruidavets, J.-B., Amouyel, P. (2003). Fish Consumption Is Associated
With Lower Heart Rates. Circulation 108: 820-825
[Abstract] [Full Text] - Lincoln, J. E (2003).
Alternate Healthy Eating Index. Am. J. Clin.
Nutr. 78: 349-349
[Full Text] - Lee, K.W., Lip, G.Y.H.
(2003). The role of omega-3 fatty acids in the secondary prevention of
cardiovascular disease. QJM 96: 465-480
[Abstract] [Full Text] - Erkkila,
A. T, Lehto, S., Pyorala,
K., Uusitupa, M. I. (2003). n-3 Fatty acids and
5-y risks of death and cardiovascular disease events in patients with
coronary artery disease. Am. J. Clin. Nutr. 78: 65-71
[Abstract] [Full Text] - Leaf, A., Kang, J. X., Xiao,
Y.-F., Billman, G. E. (2003). Clinical
Prevention of Sudden Cardiac Death by n-3 Polyunsaturated Fatty Acids and
Mechanism of Prevention of Arrhythmias by n-3 Fish Oils. Circulation
107: 2646-2652
[Full Text] - Siscovick,
D. S., Lemaitre, R. N., Mozaffarian,
D. (2003). The Fish Story: A Diet-Heart Hypothesis With Clinical
Implications: n-3 Polyunsaturated Fatty Acids, Myocardial Vulnerability,
and Sudden Death. Circulation 107: 2632-2634
[Full Text] - Albert, C. M., Chae, C. U., Grodstein, F.,
Rose, L. M., Rexrode, K. M., Ruskin, J. N., Stampfer, M. J., Manson, J. E. (2003). Prospective
Study of Sudden Cardiac Death Among Women in the United States. Circulation
107: 2096-2101
[Abstract] [Full Text] - Hu,
F. B., Cho, E., Rexrode,
K. M., Albert, C. M., Manson, J. E. (2003). Fish and Long-Chain {omega}-3
Fatty Acid Intake and Risk of Coronary Heart Disease and Total Mortality
in Diabetic Women. Circulation 107: 1852-1857
[Abstract] [Full Text] - Ziouzenkova,
O., Perrey, S., Asatryan,
L., Hwang, J., MacNaul, K. L., Moller, D. E., Rader, D. J., Sevanian,
A., Zechner, R., Hoefler,
G., Plutzky, J. (2003). Lipolysis
of triglyceride-rich lipoproteins generates PPAR ligands:
Evidence for an antiinflammatory role for
lipoprotein lipase. Proc. Natl. Acad. Sci.
U. S. A. 100: 2730-2735
[Abstract] [Full Text] - Kris-Etherton,
P. M., Harris, W. S., Appel, L. J., for the
Nutrition Committee, (2003). Fish Consumption, Fish Oil, Omega-3 Fatty
Acids, and Cardiovascular Disease. Arterioscler
Thromb Vasc Biol 23: e20-30
[Full Text] - Grodstein,
F., Clarkson, T. B., Manson, J. E. (2003). Understanding the Divergent
Data on Postmenopausal Hormone Therapy. N Engl
J Med 348: 645-650
[Full Text] - Hu,
F. B., Willett, W. C. (2002). Optimal Diets for Prevention of Coronary
Heart Disease. JAMA 288: 2569-2578
[Abstract] [Full Text] - Lemaitre,
R. N, King, I. B, Mozaffarian, D., Kuller, L. H, Tracy, R. P, Siscovick,
D. S (2003). n-3 Polyunsaturated fatty acids, fatal ischemic heart
disease, and nonfatal myocardial infarction in older adults: the
Cardiovascular Health Study. Am. J. Clin. Nutr. 77: 319-325
[Abstract] [Full Text] - Harris, W. S (2003). n-3
Long-chain polyunsaturated fatty acids reduce risk of coronary heart
disease death: extending the evidence to the elderly. Am. J. Clin. Nutr. 77: 279-280
[Full Text] - Morley, J. E. (2003).
Editorial: Hot Topics in Geriatrics. J Gerontol
A Biol Sci Med Sci 58: M30-36
[Full Text] - (2003). OMEGA-3 FATTY ACIDS
LINKED WITH LOWER SUDDEN DEATH AND CHD RISKS. Journal Watch Cardiology
2003: 5-5
[Full Text] - Guallar,
E., Sanz-Gallardo, M. I., Veer, P. v.'t, Bode, P., Aro, A.,
Gomez-Aracena, J., Kark,
J. D., Riemersma, R. A., Martin-Moreno, J. M., Kok, F. J., the Heavy Metals and Myocardial Infarction
Study G, (2002). Mercury, Fish Oils, and the Risk of Myocardial
Infarction. N Engl J Med 347: 1747-1754
[Abstract] [Full Text] - Kris-Etherton,
P. M., Harris, W. S., Appel, L. J., for the
Nutrition Committee, (2002). Fish Consumption, Fish Oil, Omega-3 Fatty
Acids, and Cardiovascular Disease. Circulation 106: 2747-2757
[Full Text] - Serhan,
C. N., Hong, S., Gronert, K., Colgan, S. P., Devchand, P.
R., Mirick, G., Moussignac,
R.-L. (2002). Resolvins: A Family of Bioactive
Products of Omega-3 Fatty Acid Transformation Circuits Initiated by
Aspirin Treatment that Counter Proinflammation
Signals. J. Exp. Med. 196: 1025-1037
[Abstract] [Full Text] - Geelen,
A., Brouwer, I. A., Zock,
P. L., Kors, J. A., Swenne,
C. A., Katan, M. B., Schouten,
E. G. (2002). (n-3) Fatty Acids Do Not Affect Electrocardiographic
Characteristics of Healthy Men and Women. J. Nutr.
132: 3051-3054
[Abstract] [Full Text] - Henriques,
J. P.S., Zijlstra, F., Siguel,
E., Hrdy, D. B., Knecht,
T. P., Albert, C. M., Stampfer, M. J., Ma, J.,
Rosenberg, I. H. (2002). n-3 Fatty Acids and the Risk of Sudden Death. N
Engl J Med 347: 531-533
[Full Text] - (2002). Omega-3 Fatty Acids
Linked with Lower Sudden Death and CHD Risks. Journal Watch Cardiology
2002: 1-1
[Full Text]
|
HOME | SEARCH | CURRENT ISSUE | PAST ISSUES | COLLECTIONS | HELP Comments and questions? Please contact us. The |