|
|
First of all, the graph implies that
risk increases steadily from 20% at 200mg% to 90% at 300mg%, but this must be
squared with the findings of Dr Carl
Seltzer who showed there were virtually identical death rates for the range
of values between 205mg% and 264mg% at the study=s 30th year. Perhaps the risk rises steeply beyond 264mg% but
since only 3% of the Framingham population were over 300mg%, it=s not of great import (unless, of
course, it’s your cholesterol that’s around 300mg%!).
Where the curves cross, at about 240,
the cholesterol levels of those with CAD is the same as the cholesterol level
of those who are CAD-free, so in this region cholesterol level has no
predictive value whatsoever! But let=s say our cholesterol is between 212
(the average for the disease-free group) and 225 (the average for those with
Coronary Artery Disease), where most of us are.
The question is: which curve are we on? The answer is: We don=t know!
Until we bite the big one, if
we bite the big one, we simply cannot tell.
So far as this data goes, it=s magical thinking to expect a change
in our chances by manipulating our cholesterol level, and this is implicit in
the statistic that half of all heart
attacks occur in people with normal cholesterol levels. In other words, it may be worth messing with
your cholesterol level if it=s around 300, but even if you get it down, you still
have a 40% chance of death from coronary artery disease!
Cholesterol risk factors don’t even predict heart disease very well!
Analysis of the
But let=s say you buy the hype, and you want
to work with your doctor to lower your cholesterol. He puts you on the National Cholesterol
Education Program “prudent diet.” But
the
|
|
Cholesterol Intake |
Blood Cholesterol Low Intake |
Blood Cholesterol High Intake |
|
Men |
483 to 925 mg |
231 mg/dl |
231 mg/dl |
|
Women |
322 to 662 mg |
251 mg/dl |
235 mg/dl |
It is crystal clear that cholesterol in the diet has no effect on blood
cholesterol!
Lowering cholesterol has never been shown to reduce the incidence of
heart disease. In an interesting meta-analysis of all the 26
cholesterol-lowering trials prior to the advent of statin drugs, about 60,000
people had their cholesterol lowered by various means, and the incidence of
heart disease among them was compared with the rate in about 54,000 people who
made no attempt to change their cholesterol level:
|
|
Treatment groups |
Control groups |
|
Nonfatal heart attacks |
2.8% |
3.1% |
|
Fatal heart attacks |
2.9% |
2.9% |
|
Total deaths |
6.1% |
5.8% |
(Ravnskov U, BMJ 1992, 305:15-9)
There were only 0.3% fewer nonfatal heart attacks, the same number of
fatal heart attacks, and 0.3% more
deaths from all causes in the treatment groups!
Even the 0.3%
reduction in nonfatal heart is probably due to chance because there were more such heart attacks in the treatment
groups in the longer trials than there were in the shorter trial, and you would
expect fewer heart attacks in the longer trials because of the lesser exposure
to high cholesterol levels. The analysis
concludes:
Lowering serum cholesterol concentrations does not reduce mortality and is unlikely to prevent coronary heart disease. Claims of the opposite are based on preferential citation of supportive trials.
Notwithstanding, the first
prescription for those at risk of CHD is the Therapeutic Lifestyle Change diet
which is designed to lower cholesterol levels by avoiding saturated fat and
replacing it with vegetable oils, and avoiding cholesterol-containing
foods. Never mind that in the Tecumseh
Study, which evaluated the effect of cholesterol, fat and saturated fat on
the blood level of cholesterol, saturated fat was found to have no effect
whatsoever on cholesterol levels:
|
Intake of: |
Blood Cholesterol Lowest third: |
Blood Cholesterol Middle third: |
Blood Cholesterol Highest third: |
|
Cholesterol |
554 mg |
566 mg |
533 mg |
|
Saturated fat |
52 mg |
52 mg |
54 mg |
|
Total fat |
128 mg |
134 mg |
133 mg |
The Table shows that the average
intake of saturated fat was virtually identical in the groups with low, medium
and high cholesterol! Further, the
average intake of cholesterol-containing foods was also virtually identical in the
groups with low, medium and high cholesterol.
This means that cholesterol in the diet has not effect on cholesterol in
the bloodstream! The study concluded that “Serum cholesterol and triglyceride
values were not positively correlated with selection of dietary constituents.”
In other words, there is absolutely no
relationship here between saturated fat, total fat or cholesterol consumption
and blood cholesterol!
But this shouldn’t really come as a
surprise. Here=s what Ancel Keys, author of The Seven Countries Study which kicked
off the whole lunatic cholesterol fiasco, had to say:

In
the adult man the serum cholesterol level is essentially independent of the
cholesterol intake over the whole range of human diets. (1956)
There=s no connection whatsoever between
cholesterol in food and cholesterol in blood.
And we=ve known that all along. Cholesterol in the diet doesn=t matter at all unless you happen to be
a chicken or a rabbit. (1997)
Key=s thrust was that fat consumption caused high cholesterol
in the blood, which caused heart disease.
However, this hypothesis is as defective as the cholesterol-in-the-diet
idea. Keys cherry-picked data from six
countries which seemed to show this relationship, but when Uffe Ravnskov plotted the data for
all the countries for which data was available, you can see that the
relationship is actually weak:
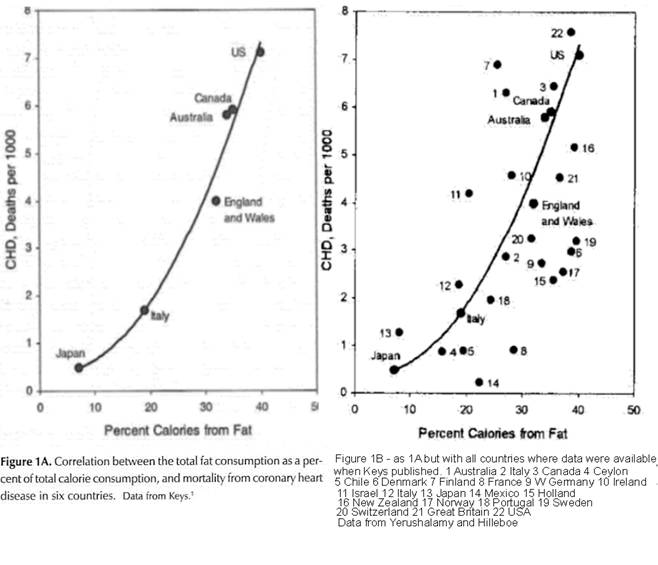
Needless to say, cherry-picking your data to show relationships you
believe to exist, but which your data does not support, is deeply bogus.
So the prescribed diet, which has those at risk of CHD avoiding saturated
fat and cholesterol-containing foods in order to lower blood cholesterol level,
cannot succeed in lowering the blood cholesterol level!
The guidelines say that the diet should be tried for three months, and
if it is without effect, then medications should be employed. But it
is a lead-pipe cinch that the diet will fail! It seems to me that the purpose of the whole
exercise is to avoid the criticism that lifestyle changes were not tried before
a drug program was instituted.
The 2002 National Heart, Lung and
Blood Institute report on Detection,
Evaluation and Treatment of High Blood Cholesterol in Adults actually
acknowledges this, and abandon cholesterol for LDL-cholesterol:
Dietary cholesterol causes marked hypercholesterolemia in many laboratory animals, including non-human primates. High intakes of cholesterol in humans, however, do not cause such a marked increase in serum cholesterol. Nonetheless, controlled metabolic studies in humans indicate that high cholesterol intakes raise LDL cholesterol. The degree of rise varies from person to person as is true for all nutrients. Meta-analysis of studies done in controlled settings confirm the LDL-raising action of dietary cholesterol.(652,653). (page V-9 of the 3rd Report of the National Cholesterol Education Program Expert Panel on Detection, Evaluation and Treatment of High Blood Cholesterol in Adults)
Uh-oh.
The studies cited are meta-analyses, statistical manipulations of
pooled studies which are only used when weak
associations need to be teased out of data with mathematical techniques!
Meta‑analysis, by promising a precise and definite answer when the magnitude of the underlying risks are small or when the results from individual studies disagree, seems an attractive proposition both in aetiological studies and in observational effectiveness research. (Spurious precision? Meta‑analysis of observational studies, Egger M et al, BMJ 1998; 7124(316))
The two studies are: Dietary lipids and blood cholesterol: Quantitative meta-analysis of metabolic ward
studies (Clarke R et al, BMJ 1987; 314:112-7), and Effects of dietary cholesterol on serum
cholesterol: a meta-analysis and review (Hopkins PN, Am
J Clin Nutr 1992; 55:1060-70). The conclusion of Clarke=s meta-analysis was that, in typical
British diets, replacing 60% of
saturated fats by other fats, and avoiding 60%
of dietary cholesterol, would reduce LDL-cholesterol by 8-12%. Such a drastic dietary change for such a
small reduction in LDL-cholesterol levels seems hard to justify, especially
when you consider that there is only an
association between LDL-cholesterol and heart disease, and there is still a
big question whether LDL-cholesterol really is a threat to the heart. Dr Uffe
Ravnskov reviewed the studies cited by the NHLBI in support of the
LDL-cholesterol – heart disease link, and pointed out that:
In
conclusion, the @large
body of evidence@ [of the
harmful nature of LDL-cholesterol] was cooked down to one single study, which
showed a predictive value for LDL‑cholesterol but for a few age groups
only. LDL‑cholesterol is neither centrally nor causally important, it has
not the strongest and most consistent relationship to risk of CHD, it has not a
direct relationship to the rate of CHD, and it has not been studied in more
than a dozen randomized trials. (Read
the complete Uffe
Ravnskov excerpt from The Cholesterol
Myths)
The “one single study”
showed LDL-cholesterol was “predictive for heart disease, but only for men
between 35 and 49 and for women between 40 and 44.” In other words, the National Research Council=s massive review of the evidence in
support of the LDL-heart disease link cited many studies which either did not
support any such link, or didn’t discuss the issue at all! Dr Ravsnkov is saying, in effect, that the
LDL-cholesterol-causes-heart-disease notion is supported by very little beyond
breathtaking, outright scientific fraud.
In his book The Cholesterol Myths (New Trends,
Our
ancestors did not know better because they had only the naked eye and lacked
the technology needed to discover the truth.
But the proponents of the diet-heart idea ought to know. Instead, their cocksure writings demonstrate
that for them the idea has become a fact, the cholesterol Earth is flat. Or is it only a game? Those of you who read this book will realize
that scientists who support the diet-heart idea and who are honest must be
ignorant, either because they have failed to understand what they have read or
else, by blindly following the authorities, they have failed to check the
accuracy of the studies written by those authorities. But some scientists must surely have realized
that the diet-heart idea is impossible and yet, for various reasons, have
chosen to keep the idea alive.
LDL-cholesterol: "Bad" Cholesterol or Bad Science?
Anthony Colpo
It is almost unprecedented for an
article to be published in The Journal of
American Physicians and Surgeons by anyone who is not an MD, yet Anthony Colpo, a fitness consultant, wrote this article. In it, he reviews the evidence, or rather the
lack of evidence, that LDL-cholesterol is a risk factor for heart disease. Incredibly,
like cholesterol, LDL-cholesterol has gained its reputation from studies which
quote studies which do not actually support the contention that LDL-cholesterol
is dangerous to the heart!
In other words it’s of marginal
value, yet has LDL-cholesterol become
the exclusive focus of the heart disease prevention and even of its
treatment! No wonder that the incidence
of heart disease continues to rise (although deaths have remained at the 1970
level, probably because of improved surgical treatments). As we shall see, oxidized LDL-cholesterol is
atherogenic – but the presence of
oxidized LDL-cholesterol is a marker for deficiencies of antioxidant vitamins
and minerals. So cholesterol and
saturated fat in the diet have little effect on blood cholesterol.
This might just be an entertaining walk
on the wild side where the loonies rant, but he is not alone. Dr Edward Pinkney
sounded such a warning in The
Cholesterol Controversy in 1978, Dr Russell Smith wrote The
Cholesterol Conspiracy in 1991,
pioneer Framingham Study researcher Dr George V Mann published Coronary
Heart Disease: The Dietary Sense and Nonsense in 1993, which was
followed by Dr Uffe Ravsnkov’s The
Cholesterol Myths in 2000, just to hit the nigh notes. Most recently, LDL Cholesterol:
"Bad" Cholesterol or Bad Science? (J Am Physicians & Surgeons 2005; 10(3)) is an admirably clear
summary of the evidence to date which exonerates LDL-cholesterol.
Apparently, the loonies doing the ranting here are members of the
American medical establishment. So how
did cholesterol become the villain?
Apparently, this came to be through
the political process!
There is no nonsense too arrant
to become policy with sufficient interference by the government
Bertrand Russel
In (Science
Science by committee
Like the flourishing American affinity for alternative medicine, an antifat movement evolved independently of science in the 1960s. It was fed by distrust of the establishment--in this case, both the medical establishment and the food industry--and by
counterculture attacks on excessive consumption, whether manifested in gas-guzzling cars or the classic American cuisine of bacon and eggs and marbled steaks. And while the data on fat and health remained ambiguous and the scientific community polarized, the deadlock was broken not by any new science, but by politicians. It was Senator George McGovern's bipartisan, non-legislative Select Committee on Nutrition and Human Needs - and, to be precise, a handful of McGovern's staff members--that almost single-handedly changed nutritional policy in this country and initiated the process of turning the dietary fat hypothesis into dogma. … McGovern and his fellow senators--all middle-aged men worried about their girth and their health--signed on; McGovern and his wife had both gone through diet-guru Nathan Pritikin's very low fat diet and exercise program. McGovern quit the program early, but Pritikin remained a major influence on his thinking.
McGovern's
committee listened to 2 days of testimony on diet and disease in July 1976.
Then resident wordsmith Nick Mottern, a former labor
reporter for The Providence Journal, was assigned the task of researching and
writing the first "Dietary Goals for the
industry as akin to the tobacco industry in its willingness to suppress scientific truth in the interests of profits. …
Creating "consensus"
Once politicians, the press, and the public had decided dietary fat policy, the science was left to catch up. In the early 1970s, when NIH opted to forgo a $1 billion trial that might be definitive and instead fund a half-dozen studies at one-third the cost, everyone hoped these smaller trials would be sufficiently persuasive to conclude that low-fat diets prolong
lives. The results were published between 1980 and 1984.
Four of these trials, comparing heart disease rates and diet within
The
sixth study was the $140 million Lipid Research Clinics (LRC) Coronary Primary
Prevention Trial, led by NHLBI administrator Basil Rifkind
and biochemist Daniel Steinberg of the
during the seven-plus years of the study was reduced
from 8.6% in the placebo group to 7.0%; the probability of dying from a heart
attack dropped from 2.0% to 1.6%.)
So this enormous dietary experiment
lessened heart risk by less than a
quarter of one percent for each year of the study, yet, incredibly, study
director Basil Rifkind suggests that the results
"strongly indicate that the more you lower cholesterol and fat in your
diet, the more you reduce your risk of heart disease." Dr Scott Grundy, a
Professor at
Grundy also writes in his letter that lowering serum LDL cholesterol by dietary means reduces CHD risk. But the study he cites did not specifically address this question (15), and more to the point, meta-analyses of all controlled and randomized trials that have used modification of dietary fat as the only type of intervention have shown that neither the incidence of nonfatal CHD, nor coronary or total mortality, was lowered significantly (16, 17).
Grundy's way of presenting scientific data is not unique. An analysis of three influential reviews in this field showed that insignificant findings in favor of the diet-heart connection were systematically inflated, and unsupportive studies were either not included or they were quoted as if they were supportive (18).
This is incredible. Tactics like these are used by Creationists
trying to refute the Theory of Evolution!
I see that the cholesterol-heart disease idea is a belief system, an
article of faith. There is no science
behind it, just the strong conviction of some that fats are harmful. You can see how funding only the research proposals of these “true believers” has got us to the
national cholesterol delusional state we are in today.
For what a man had rather
were true he more readily believes
Francis Bacon
And other than that, Mrs. Lincoln, how did you enjoy the play?
Violent death and suicide increase in
the treatment groups of the cholesterol-lowering trials. This effect is so reliable that s
meta-analysis of 6 cholesterol-lowering trials found that:
Mortality from coronary heart disease tended to be lower in men receiving interventions to reduce cholesterol concentrations compared with mortality in control subjects (p = 0.06), although total mortality was not affected by treatment. No consistent relation was found between reduction of cholesterol concentrations and mortality from cancer, but there was a significant increase in deaths not related to illness (deaths from accidents, suicide, or violence) in groups receiving treatment to lower cholesterol concentrations relative to controls (p = 0.004). (Muldoon MF et al, Lowering cholesterol concentrations and mortality. BMJ 1990; 301:309-14)
The author of this study points out that low blood cholesterol levels are most often seen in criminals, people with diagnoses of violent or aggressive-conduct disorders, homicidal offenders with histories of violence and suicide attempts related to alcohol; and people with poorly internalized social norm and low self-control.
A
prospective study in
A strong negative relation between cholesterol concentration and mortality from injuries was found in men during the first seven years of follow up. The relative risk in the lowest 25% of the cholesterol distribution was 2.8 (95% confidence interval 1.52 to 4.96) compared with the top 25%. Most of the excess risk was caused by suicide with a corresponding relative risk of 4.2 (p for trend = 0.001). (Lindberg G et al, Low serum cholesterol concentration and short term mortality from injuries in men and women. BMJ 8/1/1992; 305:277-9)
A 1998 review of all the cholesterol
lowering trials between 1965 and 1995 found the effect so strong as to conclude
that low cholesterol causes violent
behavior:
A
significant association between low or lowered cholesterol levels and violence
is found across many types of studies. Data on this association conform to
Hill's criteria for a causal association. (Golomb G,
Cholesterol and violence: is there a connection? Ann Int Med
3/15/1998; 128(6):478-87)
I’m afraid we’re seeing the tip on an
iceberg here. Many who lower their
cholesterol with statins and the AHA low-fat diet feel dreadful, but
rationalize it as due to aging, life circumstances or whatever. And many I have talked to are too frightened to make the experiment of
letting their cholesterol find its own level.
This is a dreadful human tragedy which I fear will only be appreciated
in retrospect.
The gang who
can=t shoot straight
Ancel Keys, Robert Levy, William Castelli, Antonio Gotto, Jeremiah
Stamler, Mark Hegsted, Basil Rifkind,
Scott Grundy, William Kannel – names from the small
group of cholesterol zealots who simply disregard each failed trial, declaring
them successes, and embark on yet larger studies, each of which fail in their
turn. MRFIT ($115m), LRC ($140m), ALLHAT
($125m) and the other cholesterol trials all produced trivial risk improvements
which were spun into public-relations triumphs.
In any other field of scientific endeavor, their derisory results would
spell doom for the approach, but somehow they emerge with the funding for the
next, larger, more expensive, even more lunatic
trial. It beggars the imagination.
The luck of the nine blind bastards
Australian slang meaning >very lucky indeed=
Then, lo, by a miracle, the statin drugs
appeared, which both lower cholesterol and reduce heart deaths by the unrelated
mechanism of decreasing inflammation, albeit only slightly (as in the 0.16% per
year risk reduction in the Scandinavian Simvastatin
study). If they can spin cholesterol thin
air into the appearance of success, what will they do with statins? The
answer is that they suggest that statin drugs be used for ‘prevention’ in
previously healthy persons, such as myself!
The true unimportance of cholesterol
levels
Remember also that in 1900, heart
attacks were so rare that they weren=t recognized as a cause of death, and
cholesterol levels have not much changed since then. Furthermore, people with very high
cholesterol levels caused by a genetic condition called familial hypercholesterolemia did not die prematurely of heart
disease in 1900, although they do now:
Mortality was
not increased in carriers of the mutation during the 19th and early 20th
century; it rose after 1915, reached its maximum between 1935 and 1964
(standardized mortality ratio 1.78, 95% confidence interval 1.13 to 2.76;
P=0.003), and fell thereafter. (Sijbrands
EJG et al, Mortality over two centuries in large pedigree with familial
hypercholesterolemia: family tree mortality study. BMJ
2001; 322:1019‑23)
This suggests environmental
factors absent in 1900 and in place by 1915 increased heart attack
deaths. The vitamin and mineral content
of the American diet fell precipitously during this period as the use of sugar
and bleached white flour became widespread, and trans-fats were introduced with Crisco in 1911.
I=m reminded of another conclusion of
the
From
1951 to 1955 serum cholesterol levels were measured in 1959 men and 2415 women
aged between 31 and 65 years who were free of cardiovascular disease (CVD) and
cancer. Under age 50 years, cholesterol levels are directly related with 30‑year
overall and CVD mortality; overall death increases 5% and CVD death 9% for each
10 mg/dL. After age 50 years there is no increased
overall mortality with either high or low serum cholesterol levels. There is a direct association between
falling cholesterol levels over the first 14 years and mortality over the
following 18 years (11% overall and 14% CVD death rate increase per 1 mg/dL per year drop in cholesterol levels). Under age 50
years these data suggest that having a very low cholesterol level improves
longevity. After age 50 years the association of mortality with cholesterol
values is confounded by people whose cholesterol levels are falling‑‑perhaps
due to diseases predisposing to death. (Cholesterol and mortality. 30 years of
follow‑up from the
This study is usually quoted in
support of the oft-repeated
statement that each “1% reduction in an individual's total serum
cholesterol level translates into an approximate 2% reduction in CHD risk.”
However, I can’t find anything in
this study which even remotely supports this, but maybe,
just maybe it’s true for those under 47 years of age. However, I=m 59, so my cholesterol has bugger all to do with my risk of CVD. In fact, I’m at 99% greater risk of mortality over the next 18 years because my
cholesterol level fell from 275 to 165 between 1983 and 2003 (a fall of 110),
and further reduction would seem to increase
this risk! Yet the guidelines suggest a statin and a diet to lower my already low cholesterol even though the study on which the
recommendations are supposedly based found that falling cholesterol predicts death!
That low cholesterol predicts death
is not an orphan finding. For example,
the Honolulu Heart Study concluded:
AA generally held belief is that
cholesterol concentrations should be kept low to lessen the risk of
cardiovascular disease. However, studies of the relation between serum
cholesterol and all-cause mortality in elderly people have shown contrasting
results. Y Methods Lipid and serum cholesterol
concentrations were measured in 3572 Japanese/American men (aged 71-93 years) as
part of the Honolulu Heart Program. We compared changes in these concentrations
over 20 years with all-cause mortality using three different Cox proportional
hazards models. Findings Mean cholesterol fell significantly with
increasing age. Age-adjusted mortality rates were 68.3, 48.9, 41.1, and 43.3
for the first to fourth quartiles of cholesterol concentrations, respectively.
Relative risks for mortality were 0.72 (95% Cl
0-60-0-87), 0.60 (0-49-0-74), and 0.65 (0-53-0-80), in the second, third, and
fourth quartiles, respectively, with quartile 1 as reference. A Cox
proportional hazard model assessed changes in cholesterol concentrations
between examinations three and four. Only the group with low cholesterol
concentration at both examinations had a significant association with mortality
(risk ratio 1.64, 95% Cl 1.13-2.36). Interpretation We have been unable to explain our results. These data cast doubt on
the scientific justification for lowering cholesterol to very low
concentrations (<4.65 mmol/L) in elderly people. (Schatz I et al, Cholesterol and
all-cause mortality in elderly people from the Honolulu Heart Program: a cohort
study. Lancet 2001; 358: 351-55)
Translation: People over 72 with low
cholesterol were at considerably greater risk of death than those with high
cholesterol, and falling cholesterol apparently heralds approaching death. I=m left with this thought from Dr
William Castelli, Director of the Framingham Heart
Study at the time, that:
In
Framingham, Massachusetts, the more saturated fat one ate, the more cholesterol
one ate, the more calories one ate, the lower people's serum cholesterol ... we
found that the people who ate the most cholesterol, ate the most saturated fat,
ate the most calories weighed the least and were the most physically active.
... In view of this, this study fails to describe a relationship of those
traditional dietary constituents, saturated fat and cholesterol, known to have
an adverse effect on blood lipids, and thereby, on the subsequent development
of coronary disease end points. (Castelli WP, Concerning the possibility of a nut ... Arch Intern Med 1992; 152:1371‑2)