The exhaustion of iodine in the soil and our failure to add
it to fertilizer, and the widespread distribution of goitrogens (substances
which interfere with thyroid metabolism) such as fluoride, chlorine and soy
products, has caused a massive, unrecognized depletion of iodine in the
citizens of America. Iodine is added to
table salt. In 1924, the incidence of
goiter amongst
A prominent use for iodine in the body is the production of thyroid
hormone, essential for energy production in every cell of the body. The physician Broda Barnes estimated that 40%
of the population had hypothyroid symptoms in 1966. A contemporary physician, Dr David Brownstein, estimates
the incidence at 30-40%, and there is laboratory evidence of thyroid disease in
10%. However, these physicians maintain
that it is widely misdiagnosed because the symptoms are so diverse, and because
the laboratory tests are unreliable.
Hypothyroid symptoms may include ...
Circulation Appearance
Atherosclerosis,
maybe with: Dry
skin, brittle nails
Cold
hands, feet, cold intolerance Hair
loss
High
or low blood pressure Puffy
eyes, eyelids
Slow
heart beat Demeanor
Edema Lethargy,
depression
Reproduction Nervousness,
irritability
Infertility
Poor
memory, concentration
Irregular
menstruation Type
A personality
PMS,
premenstrual weight gain, edema Hypoglycemia
Other
Susceptibility
to infections, addictions
Hoarseness,
slow speech
Constipation
High
cholesterol
The Recommended Dietary Allowance, when met, addresses goiter
and cretinism, but what other functions does iodine have in the body besides
supplying the raw material for thyroid hormone? Iodine and/or iodide are concentrated by
tissues of the breasts, ovaries and prostate gland. As with the thyroid gland, a deficiency of
iodine causes hyperplasia, swelling as the cells proliferate in an attempt to
garner more of the available iodine. This
causes goiter in the thyroid gland, cysts in the breasts, large breasts,
fibroid tumors, and Benign Prostatic Hypertrophy in the prostate, and
predisposes to cancer of these organs. All these conditions occur at epidemic
levels in this country.
In the face of this public health emergency, it would seem
prudent to raise the rate of supplementation, but, extraordinarily,
endocrinologists have an exaggerated fear of this course of action. They fear thyroid cancer will rise, even
though thyroid cancer is on the rise in spite of iodine intake falling for years since the baking industry
switched from iodine-based dough conditioners to bromine-based products on
fears from the National Institutes of Health that levels were too high.
Another fear, also out of the National Institutes of Health,
is of the Wolff-Chaikoff effect of thyroid suppression from excess iodine
intake which had been seen in rats and extrapolated to humans without ever
actually having been seen in humans. But
the Wolff-Chaikoff effect is supposed to begin at 200 micrograms, and since the
Japanese consume some 13.5 grams of iodine each day and have the lowest rates
of hypothyroidism, heart disease, breast, ovarian and prostate cancer in the
world, this belief clearly needs to be re-examined.
Entertainingly, a thyroid researcher, Dr Guy Abraham, has
offered $10,000 to the first physician who can show him a case of the
Wolff-Chaikoff effect in a human patient:
We have given up to 50 mg iodine/iodide
per day for up to one year to normal subjects without any ill effect. Serum T4
levels did decrease but remained within the normal range. Serum TSH decreased
in those with elevated levels, but not in subjects with TSH below 2.5 mIV/L.
We are offering $10,000 to
any physician or other health care professional who can demonstrate the Wolff
Chaikoff Effect in human subjects with normal thyroid function. (The
Wolff-Chaikoff effect of increasing iodide intake on the thyroid - Letters to
the Editor, Townsend Letter for Doctors and Patients, 12/2003; Dr Guy
Abraham)
Hypothyroidism contributes to atherosclerosis?
The observation
that hypothyroidism contributes to atherosclerosis has been made by many and
ignored by many over the years. Dr Broda
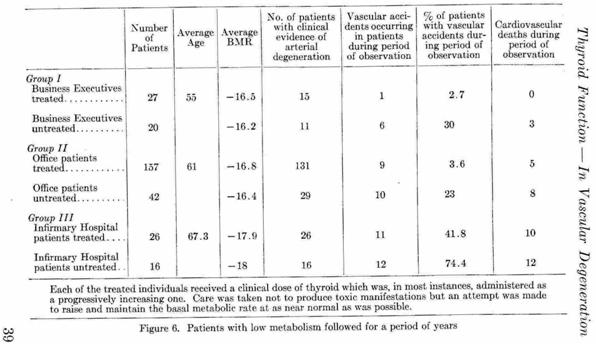
Barnes compared his thyroid-treated patient population with the
(from Barnes BO et al, Heart attack rareness in thyroid-treated patients, 1972, C Thomas IL pub)
Paul Dudley White, the cardiologist who attended President
Eisenhower after his heart attack, published a study of 28 patients under 40
who had suffered heart attacks and whose angina diminished with thyroid
treatment (White, PD et
al, Metabolic changes in young people with CHD, J Clin Invest 1946; 25:914).
Kountz published a 5-year controlled study in 1951. The results were dramatic. Two hundred and eighty eight patients were
divided into experimental and control groups with small doses of thyroid being
given to the experimental groups:
There were 11 times as many “vascular accident” in the
untreated business executives, 6 times as many in the untreated Office
patients, and almost twice as many in the highest risk group, the untreated
|
|
(From Kountz, WB. Thyroid function and its possible role in vascular degeneration. American lecture series, 1951, #108. C Thomas IL pub)
The point here is that there is a very low rate of heart disease in those treated with thyroid hormone.
Why does low thyroid predispose to heart disease? One reason may be that hypothyroid people
have elevated
homocysteine levels, known to increase heart risk by about 3 times. Treating the hypothyroid condition lowers
homocysteine to the normal range without folic acid supplementation in most
people.
A second reason may be that thyroid hormone lessens the
clotting tendency, and a third reason may be that thyroid hormone controls the
formation of the material between cells.
This is a mixture of cross-linked tendrils of collagen intermixed with
gluey stuff called glycosaminoglycans, very much as reinforced concrete is
reinforcing bars intermixed with concrete.
Such composite materials are far stronger than their components, and a
strand of collagen is as strong as the same diameter of rebar material.
However, the active form of the thyroid hormone, T3, enhances
the production of mucin
and inhibits formation of collagen,
so that the hypothyroid has too much concrete and not enough rebar. Buildings made like this are forever
collapsing in third-world countries at the first hint of an earthquake. The consequence in the arterial wall is
weakness and susceptibility to damage.
The poorly supported cells of the intima sustain damage from the force
of the blood flow or the flexing of the artery, exposing the collagen to
abrasion. As discussed elsewhere, the
abrasion of collagen exposes lysyl and prolyl residues which link to
lipoprotein(a), the “bad” LDL form of cholesterol elaborated with
apoprotein(a). This particle bridges the
tear between the collagen strands, effecting a repair of the collagen at the
expense of introducing plaque into the arterial wall.
Interestingly, mucopolysaccharides also accumulates in those
with cancer, diabetes, arthritis and hypertension which could mean some degree
of hypothyroidism contributes to or is caused by these conditions.
Certainly, there is no reliable laboratory test currently,
and there is a long history of failed tests such as that for Protein-Bound
Iodine which took decades to become discredited. This may be because most tests look at
thyroid hormone in the bloodstream, while thyroid hormone acts within the cell
after it has been converted to its active T3 form. The Thyroid Stimulating Hormone test measures
the level of the pituitary hormone which tells the thyroid to release thyroid
hormone, but it has such an enormous “normal” range that it’s essentially
useless unless the top half of the range is reclassified as “subclinical
hypothyroidism.” This category has been
forced upon endocrinologists by dissatisfied patients.
Barnes found that thyroid tests gave false negatives so often
that he instead treated the hypothyroid symptoms if the body temperature was
low. Since thyroid hormone controls the
metabolism, a shortage affects body temperature. The Barnes Basal Temperature test takes
advantage of this. The temperature in
the armpit is taken on waking for ten days, and the normal range of the average
is 97.8 to 98.2EF. This test was in the
Physicians Desk Reference for many years, and, if hypothyroid symptoms are
present, is strong evidence of a hypothyroid condition.
Pursuing this strategy, Barnes undoubtedly treated many who
had TSH above 2.5, where the new category of subclinical hypothyroidism
starts. Interestingly, the Wickham study (which is often quoted as
showing that hypothyroidism is rare, and that there is no association between
hypothyroidism and ischemic
heart disease) used a TSH of 6 as
the threshold of hypothyroidism, and, unsurprisingly, found a low incidence of
hypothyroidism and little correlation with atherosclerosis, but that the
likelihood of developing hypothyroidism was very high if the TSH was over 2 at
the start of the study:
The odds ratios (with 95% confidence intervals) of developing hypothyroidism with (a) raised serum TSH alone were 8 (3-20) for women and 44 (19-104) for men; (b) positive anti-thyroid antibodies alone were 8 (5-15) for women and 25 (10-63) for men; (c) both raised serum TSH and positive anti-thyroid antibodies were 38 (22-65) for women and 173 (81-370) for men. A logit model indicated that increasing values of serum TSH above 2mU/l at first survey increased the probability of developing hypothyroidism which was further increased in the presence of anti-thyroid antibodies. (Vanderpump MP et al, The incidence of thyroid disorders in the community: a twenty-year follow-up of the Whickham Survey. Clin Endocrinol (Oxf). 7/1995; 43(1):55-68)
(It’s not entirely clear if Vanderpump means over 2, or an
increase of 2 units over the starting value – but what the hell, what is clear
is that if you fix hypothyroidism at over 6, you miss those who are incubating
hypothyroidism.)
Since then, subclinical
hypothyroidism has been found to be associated with double the incidence of
atherosclerosis and triple the rate of heart attack in a population of elderly
women. Barnes was ahead of the
game!
The prescription for a hypothyroid condition is most often
thyroxine in the form of Synthroid.
The pharmaceutical company
that makes this drug is the main funding source of the endocrinology society,
and quite often doctors that speak at continuing educational seminars and
conventions have ties to this drug company. Also, many doctors are more willing
to write subscriptions for antidepressants when the patient complains of
feeling lethargic, statins when their cholesterol levels rise, when all that
may be needed is an increase in the dosage of thyroid hormone as well as a
different drug. Studies published in
medical journals indicating many patients have better quality of life when on
medication that contains t3 in addition to t4 are ignored or suppressed.
Last year, I read studies
that were interpreted by an endocrinology society showing synthetic t4 as the
best treatment for hypothyroidism, when in fact if one read the whole study,
and not just the edited version one would wonder how that conclusion was
reached. This is a very serious matter.
From what I have read non or under treated thyroid disease can lead to
vascular and heart disease, so wouldn't under treatment be potentially harmful?
New guidelines for TSH came
out in 2002 and yet no lab I know of is using the .02 to2 tsh as being in
range? Why is it that many doctors are
so closed minded about any other drug but synthetic t4 mention natural thyroid and they say, AWe
don't use it any longer because we have to worry about pig viruses being passed
to humans.@ They don=t seem to worry
about that when using pig valves for the heart.
Thyroxine is synthetic T4, a part of what the thyroid
secretes, and whose most dramatic property is that it normalizes thyroid test
results. Unfortunately, it often does
very little for hypothyroid symptoms. As
a psychotherapist, I have many times referred people to their physicians for
evaluation of suspected hypothyroidism because their presentation includes
depression, nervousness or some other condition which finds a home in the
list. The first hurdle is the normal
test result. After the physician is educated
about subclinical hypothyroidism, the second hurdle is Synthroid, which does
little to relieve the psychological sequelae of hypothyroidism. When I made inquiry, I learned that the
doctors were quite consistent in claiming that dessicated thyroid was
unreliable in strength and full of insect parts. Apparently, the Knoll Pharmaceutical people
made these claims to sell their Synthroid, and a very successful campaign it
was! Even after Synthroid was
practically pulled from the market by the FDA for unreliable potency (the very
thing they claimed of dessicated thyroid), doctors are still squirrely about
the Armour product because of the insect parts claim, even thought all natural
products (including oatmeal, for example) are allowed by law to contain a small
proportion of insect parts.
Unfortunately, neither Synthroid, Euthroid or Thyrolar (which contain
some T3 with T4) relieve the symptoms as well as Armour dessicated
thyroid.
I make this diversion to underline how difficult it may be
for a citizen to obtain the hypothyroid diagnosis, and be effectively
treated. The symptoms for which people
consult me are identical hypothyroid symptoms, and in some cases respond to
dessicated thyroid, but not Synthroid.
So I am in 100% agreement with Dr Guy
Abraham when he wrote:
The Wolff Chaikoff Effect, combined with medical stupidity may have caused more human misery and death than both world wars combined by preventing meaningful clinical investigations of optimal levels of iodine on physical and mental health. Today, the optimal requirement of iodine for whole body sufficiency is still unknown.
One of the few things researchers agree on is that the
initial injury in atherosclerosis is caused by the hydrodynamic stresses of
rushing blood abrading the aorta, or is from a mechanical stress of the
coronary arteries from the heartbeat, as might be the case if the ground
substance is weakened.
Animals whose thyroid glands are removed rapidly develop
atherosclerosis. Parenthetically,
cholesterol fed to herbivores suppresses their thyroid function, so the
atherosclerosis of Anitschkow’s famous cholesterol-fed rabbits (which
contributed so much to the cholesterol scare) was not due to the oxidized
cholesterol in their feed may have been due to their hypothyroid state. Low thyroid leaves one vulnerable to
infection, and infectious diseases cause the rapid progression of
atherosclerosis. As early as 1919, it
was noticed that those dying of tuberculosis had atherosclerosis considerably
more advanced than their age would suggest, and in 1925 children as young as 6
months of age who died of infectious diseases showed atheromatous arteries at
autopsy (Zinzerling, WD, Researches on atherosclerosis: on the aorta fat in
children. Virchows Arch Path Anat 1925; 225:677) Recently, childhood
inflammation (such as that which would be experienced during childhood
infections) was shown to be a predictor of early death in a pre-antibiotic
population; and the hypothyroid state is known to be one of high
oxidative stress, that is, inflamed.
Could it be that it is lifelong hypothyroidism which causes early death?