Hypoglycemia & Neurosis
I treat neurosis according to the methods of Dr Arthur Janov. Briefly, if neurotic behavior is the symbolic recreation of childhood trauma, then the neurotic tries to fulfill old, unmet needs in present relationships. The consequent suffering and confusion is relieved only when he or she relives the childhood distress in its true context during deep feeling events called Primals.
Pondering the slow progress of a patient, I realized with amazement that his symptoms were what I experience when I've taken too much insulin to treat my diabetes - he was hypoglycemic! I had thought of hypoglycemia as a discredited sixties fad, but have learned that this is not so. Hypoglycemia means low blood sugar, and it can be caused, paradoxically, by high levels of sugar in the diet (Hofeldt 1989). Measures which stabilize blood sugar also stabilize mood, and make the therapeutic process infinitely easier. Low blood sugar, on the other hand, can make life a misery. Once my suspicion was aroused, I noticed others with hypoglycemic symptoms.
§§
I saw an executive dietician who felt she was in danger of losing her job because of temper outbursts. She felt "unstable" and shaky under pressure. A vegetarian, she wrote "I mostly drink coffee with 2 sugars for breakfast, and eat cooked vegetables with pasta for lunch. I eat a lot of green salads and vegetables for dinner, with tofu as my main protein source. I've had several episodes of low blood sugar. Once, when I was feeling particularly terrible before dinner, I took my blood sugar. It was much too low at 58 mg/dl. This was after a very emotionally distressing day."
Her MD husband is also vegetarian. He would have episodes of anhedonia (loss of all pleasure in life) and agitated depression so profound that he contemplated suicide. He ate a great deal of fruit, and ate nothing but fruit for breakfast.
A sculptor often collapsed from exertion into "a catatonic state for minutes or hours, able to hear but unable to move a muscle or even open my eyes. I experienced a sense of depersonalization, and radical mood swings triggered by almost anything." Three doctors gave him a clean bill of health, and one advised him to "come back when you're worse." He thought he was dying of an unknown tropical disease, so he put his affairs in order. His wife had just given birth to a daughter. His distress was acute. He ate tropical fruit and drank a great deal of fruit juice.
A musician's episodes of depersonalization and delusional perceptual shifts were so disturbing he couldn't work. Perceiving his girlfriend as male caused him to panic. When he remembered to eat, he ate breakfast cereal and bananas.
An overweight
His wife, a Marriage, Family and Child Counselor, had suffered migraine headaches on waking for many years.
Another MFCC overworked compulsively because he felt he couldn't fulfill his obligations to patients, fiancé and family. A life-long insomniac, he took Dalmane, Soma and Ativan to get to sleep, but woke in the early hours. He ate little in the day, and raided the cookie jar when he got home in the evening. His blood sugar was 55 mg% on waking, and 64mg% when he got home.
§
I myself am an insulin-dependent diabetic,
and have experienced hypoglycemic symptoms caused by too much insulin. I knew
from firsthand experience that in hypoglycemia, "any aspect of the entire
range of neurologic or psychiatric disorders may be
mimicked, including ... outbursts of temper, extreme depression, or apparent
catatonic schizophrenia" (
§
The executive dietician has been too busy to address the issue thoroughly. She wrote that "My diet is still sweet, but that is just where I am at now. Every day is a new day, so we will see."
Her husband, the vegetarian MD, wrote that "I'm eating more protein early in the day, and I'm hungry in the morning again - how does that work exactly? I feel way more stable, have about 95% less flatulence, and my sex drive is way up!" His anhedonia and depression have not recurred.
The sculptor wrote that on changing to a high-protein, Atkins-style diet, "within hours I began to feel stronger. The cramps disappeared soon after and the dizziness dissipated. I'm back at work. I notice that my allergies, which had become extremely severe along with the general decline in my health, disappeared immediately. Second, irritable bowel syndrome was eliminated in two weeks. Finally, my migraine headaches of the last 25 years have dropped off almost entirely."
The musician's perceptions are more stable and he's back at work. In his words, he's "hanging in there." The extent of his dietary improvement was a migration from cereal to Egg McMuffins for breakfast, but even this was enough to resolve the worst of his symptoms.
The
His wife took up the diet with him, and she reports that her long-time migraine headaches are 95% resolved (except when she eats chocolate). She has halved her dose of Prozac, and troublesome "out of focus" feelings during clinical interviews have ceased.
The workaholic MFCC recognized that his mood swings were caused by hypoglycemia, and believes he has been hypoglycemic since early childhood. He eats more regularly, and has switched from his usual snack bar which contained the equivalent of seven teaspoons of sugar to a brand with much less. He is going on a much-needed six-month sabbatical.
§
Hypoglycemia is said to be "uncommon, if not rare," but it is clearly not rare in my practice. In trying to refer these patients to physicians for Glucose Tolerance Tests, I found that "skepticism and even frank disbelief exist among some medical authorities regarding the very existence of ... reactive hypoglycemia" (Hofeldt 1989).
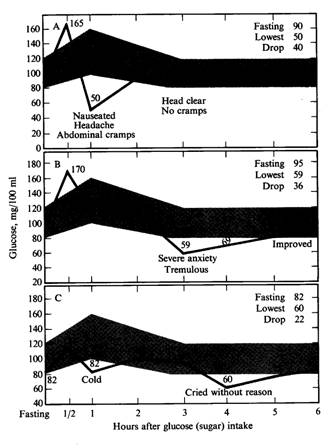
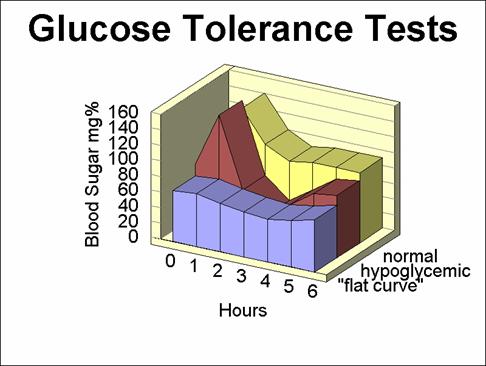
In the Glucose Tolerance Test, 50-100 grams of glucose is given to a fasting patient whose blood sugar is taken every half-hour or hour for the next two hours to discover diabetes, or for 5-6 hours to diagnose hypoglycemia. Hypoglycemia is considered to be present if symptoms coincide with low blood sugar, which means that hypoglycemia is overlooked if the patient doesn’t complain of symptoms. Many Glucose Tolerance Tests last only three hours and would miss hypoglycemia in the 3rd patient above.
Notwithstanding, San Francisco psychiatrist Michael Lesser found that all but eight of 97 patients diagnosed neurotic were also hypoglycemic according to the Glucose Tolerance Test. In testimony before a Congressional Select Committee on Nutrition and Mental Health, he said that "the blood sugar pattern of hypoglycemia is always present in neurosis." One third of his cases with "flat curve" hypoglycemia had the "flat, stoical, unchanging affect" of depression, while those with wide swings in blood sugar suffered more from mood swings, manic depression, and hysteria (Lesser 1980). Hysteria was attributed to "a wandering uterus" until the 19th century. Although we now know the uterus doesn't wander, Dr Lesser suggests that it is wandering blood sugar which aggravates mood-swing conditions like hysteria.
Lesser follows in the footsteps of a Dr Hoffman, who found that two hundred and twenty people entering therapy in a psychiatric practice had symptoms suggestive of hypoglycemia. Ninety-three percent had blood sugar falls to below 70mg% during the Glucose Tolerance Test. When their hypoglycemia was treated, all improved in their physical complaints and "their psychic symptoms waned and abated ... we had achieved an open sesame to those hidden and so-called sub-conscious conflicts that had hitherto presented adamantine resistance to psychiatric approach" (Hoffman 1949). Apparently, mood follows blood sugar.
§
I was surprised to learn that research has, in fact, established a cause for hypoglycemia: "reactive [meaning after a meal] hypoglycemia ... occurs primarily in individuals who consume a peculiar diet that has a high composition of refined carbohydrate calories (Hofeldt 1989). In other words, refined carbohydrates such as sugar and white flour products cause hypoglycemia.
Who is drawn to such "peculiar" diets? The answer, it seems, is those who crave relief from repressed pain and stress in their lives. Sugar somehow elicits the secretion of the body's "feel-good" endorphins, so much so that the pain threshold of baby rats almost doubles. The blood of newborn human babies is routinely sampled by heel prick, a painful procedure that usually causes crying. However, after sugar is given, the tears are brief. Beta-endorphin levels increase in binge-eaters (Blass 1987-1995, Fullerton 1985), which may be why they over-eat.
However, endorphins eventually fall in chronically sugar-fed rats, and their pain thresholds fall with them (Roane 1990). In other words, you need more and more sugar to get the same relief, until you're in Betty Crocker country and your diet has become "peculiar." This kind of "habituation" is found in all opiate-mediated addictions, including chronic alcoholism (Genazzani 1982), in which opiate-like isoquinolones are formed from a breakdown product of alcohol and the neurotransmitter dopamine.
Endorphins, our self-made opiates, have receptors in brain structures mediating emotional feelings as well as those dealing with physical sensations of pain and stress. The sense of urgency we experience with a full bladder is caused by low endorphins. Babies who are breast-fed often appear ecstatic, and this state coincides with high levels of endorphins. In adults, there are high levels of endorphins during and after orgasm. Thus, endorphins motivate as well as providing comfort and gating pain. And they are among the most addictive substances on the face of the planet. So perhaps it's not so surprising that "20 percent [of hypoglycemics] give a history of intense, insatiable and irresistible craving for sweets and carbohydrates" (Buehler 1955), while the rest are strongly attached to their "peculiar" diets. Hypoglycemics are unwittingly trying to self-medicate their profound subconscious malaise with food.
A Canadian who was diagnosed hypoglycemic years ago told me that he was left to cry for the first eight months of his life, until his mother found that sweetened condensed milk comforted him. From then on, he had vast quantities of sugar. In therapy, he realized sugar comforted the buried desolation imprinted in him by his early deprivation, and that eating too little food was a symbolic recreation of this trauma.
The seven people whose experiences are set out here have stories which are variations on this theme.
§
In researching hypoglycemia, I found three categories of symptoms of increasing severity.
First, there's "relative hypoglycemia," so-called because symptoms coincide with the blood sugar falling about 20mg% relative to the fasting level. These symptoms may happen while the blood sugar is in the normal range.
For example, a 1943 study found "weakness and hunger" two hours after a high-sugar breakfast (Thorn 1943). This and numerous studies which followed agree that high-protein, low-carbohydrate diets excluding both sugar and caffeine prevent such symptoms (Moersch 1937, Himwich 1944, Fabrikant 1955, Gyland 1957, Phillips 1959, Buehler 1962, Salzer 1966, etc). I experience "relative hypoglycemia" symptoms when my blood sugar falls rapidly, including weakness, nervousness, irritability and mental dullness. However, research into relative hypoglycemia lost momentum, perhaps because no mechanism existed to account for the symptoms. Recently, however, such a mechanism has been discovered, as we shall discuss.
The second category of symptoms stem from stress hormones secreted to raise the blood sugar when it falls below normal. One of these hormones is the fight-or-flight hormone adrenalin which affects mood dramatically, causing heightened vigilance, shaking, sweating, tremulousness, anxiety, irritability or even paranoia without any change in present circumstances. The combination of adrenalin and low blood sugar negates the comforting effect of the endorphins, so the sufferer is doubly uncomfortable. (This is familiar to insulin-dependent diabetics as a "Somogyi reaction", in which the adrenalin can drive the blood sugar to high levels after it falls below normal in an "insulin reaction.") This distress is evident to observers, and the corresponding blood sugar and stress hormone levels can be measured during the Glucose Tolerance Test, so this kind of symptom is well accepted.
The third category of symptoms is caused by "neuroglycopenia" (literally "brain-sugar-lack.") Glucose reaches the brain cells by the slow process of diffusion from the capillaries, so the brain runs out of fuel if low blood sugar persists. Incredibly, brain metabolism fell to 22% of baseline in experimental, insulin-induced hypoglycemia (Himwich 1944). The cortex suffers first, so cortical functions such as insight are the first to be affected which means that the sufferer can have little insight into the cause of the suffering. Hence, "the neurologic and psychologic symptoms [which] predominate in hypoglycemic reactions ... are so protean and variable ... [they] may masquerade ... as ... hysteria, migraine, petit mal, narcolepsy ... and even the psychoses" (Harris 1936).
In "Insulin Shock Therapy," depression was treated by inducing severe neuroglycopenia with injections of insulin. The consequent disruption of mental processes leaves a measure of amnesia behind it, rather like pushing the "reset" button on a computer.
Two of my thin hypoglycemic patients, the dietician and the musician, appeared to have neuroglycopenic symptoms more or less all day. This was likely because they ate small, sweet snacks of fruit juice or something similar all day long, just enough to cause chronic over-secretion of insulin.
While symptoms from adrenalin release are usually obvious, those from neuroglycopenia may go unnoticed because the inward state can include mental dullness, apathy and confusion while the outward appearance remains normal. This may account for the studies which deem people with low blood sugars "asymptomatic" because they appear normal when their blood sugars are low during the Glucose Tolerance Test. It would be interesting to give an IQ test at the blood sugar nadir to discover how asymptomatic these people really are. Perhaps Winnie the Pooh would not have felt himself to be "a bear of little brain" if he'd kept off the honey!
§
The combination of adrenalin and neuroglycopenia can produce a spectrum of symptoms from lethargy to rage, obstinacy, unsocial or antisocial behavior, even arson and violent aggression. Although hypoglycemia does not readily spring to mind as an explanation for such behaviors, I believe they are caused by hypoglycemia far more frequently than is generally recognized.
For example, 46% of a group of Finnish arsonists were diagnosed as hypoglycemic by the strictest criteria (Virkkunin 1984), while eight studies found "between one half and two-thirds of schizophrenic patients suffer from relative hypoglycemia" (Hawkins 1973); and it is thought to occur in 95% of alcoholics. Incredibly, 100% of a prison population of habitually violent offenders were profoundly hypoglycemic, and all had committed crimes while intoxicated (Virkkunin 1982). Alcohol deepens hypoglycemia by inhibiting the liver's ability to raise blood sugar until the alcohol has been metabolized.
§
The research which showed that refined carbohydrates cause hypoglycemia found that "symptoms did not occur when refined carbohydrates were restricted to 10-12% of ... total carbohydrate intake" (Hofeldt 1989, Sanders 1982). Hence, the remedy for hypoglycemia is to exclude refined carbohydrates from the diet. That this remedy is effective not just in extreme hypoglycemia suggests that blood sugar disturbances are much more widespread than has been supposed.
For example, reducing sugar in the diet of 174 juvenile delinquents resulted in 83% fewer assaults, with greatest effect among those charged with robbery, rape, aggravated assault, vandalism, child molestation, arson and possession of a deadly weapon (Schoenthaler 1983).
Whatever the merits of the "sugar causes hyperactivity" debate (in which some negative studies appear to have been designed to refute the hypothesis), it is incontrovertible that 803 New York City schools increased their score on the national school ranking system (the California Scholastic Aptitude Test) by an average of 15 points (a very large, statistically significant gain) when sugar was lowered to near 10% of the two school meals fed to the students daily, and that this gain was reversed when sugar was once more uncontrolled (Schoenthaler 1986). A proof-reader of this article recognized this effect in the unruly child of a friend of hers. When she encouraged her friend to restrict sugar in the child's diet, his mood swings lessened and he became more cooperative. It is apparent that hypoglycemia associated with sugar consumption contributes to society's most severe and intractable problems, including violent crime and the failure of education.
§
Hypoglycemia is caused exclusively by refined carbohydrates. Refined carbohydrates cause more insulin than necessary to be released, so that the blood sugar inevitably falls below the fasting level (causing symptoms in some people but not in others).
I was amazed to find that this is common knowledge! For example, transfusions of glucose cause hypoglycemia, so post-operative patients are closely monitored for the symptoms (JAMA 1956). An editorial on hypoglycemia acknowledged that "after ... people ... ingest glucose ... or a high carbohydrate meal, it is not uncommon that the blood sugar decreases to levels below normal ..." (JAMA 1973). However, unrefined carbohydrates such as rice do not cause the blood sugar to go below the fasting level (Crapo 1977), do not cause the release of endorphins, and do not cause hypoglycemia.
The conclusion of researchers that hypoglycemics suffer "a genetic maladaptation in the handling of carbohydrates" (Hofeldt 1989) is patently absurd. A creature cannot have any kind of "genetic adaptation" to a food unless it was available during its evolution! During the evolution of the human race, free sugars were available only in small quantities, seasonally, in honey, while all other sugars were to be found only in fruit and vegetables along with vitamins and minerals, and fiber which slows the uptake of glucose into the bloodstream. The intake of refined sugars has grown explosively to the present astounding average of 150 pounds per person per year in the past few dozen generations (USDA 1997). On an evolutionary time scale, this is but the blink of an eye. A more fitting conclusion is that refined carbohydrates, especially sugar, are a defective food because people have had so little time to adapt to them.
This may seem to go beyond the facts, but consider that sugar is acknowledged to cause tooth decay and that 98% of Americans have caries, while studies of the skulls of peoples who did not consume sugar show a caries rate of about 2% (Price 1945). Caries are maladaptive in evolution because children with rotten teeth would be less likely to survive to breeding age. The conclusion that sugar is a defective food for people is inescapable.
If sugar is a defective food, why do we have a taste for it? Probably because survival was the reward for seeking out hard-to-find fruit in the summer. The weight gained in this way would more readily permit survival in harsh winters. Remember that the human race survived many ice ages, in which the summers were brief and the winters severe. This so-called "thrifty gene" hypothesis seems to explain both our taste for sweet things and our inability to handle them.
How exactly does sugar damage teeth? It's very interesting, and not widely known, that sugar reverses the flow of dental lymph. The pulp of the tooth is extremely active metabolically, generating a high pressure which pushes lymph out of the tooth through tiny tubules in the dentin and enamel. When sugar is given, the internal pressure within the tooth falls and fluids from the mouth are drawn into the tooth. Unfortunately, these mouth fluids include the acid wastes of plaque bacteria which cause decay inside them. Thus, no amount of oral hygiene can entirely prevent sugar from causing tooth decay (Steinman 1984).
In the study which established this, the caries rate was reduced when the sugar diet was supplemented with the minerals calcium, magnesium and phosphorus. It's long been known that sugar causes these nutrients to be lost in the urine, but the calcium level in the blood hardly varies. However, recent nuclear magnetic resonance imaging studies show that the blood sugar level determines calcium and magnesium levels inside the cell. The studies found that the higher the blood sugar, the more calcium and the less magnesium there is within living cells (Barbagallo 1994).
This has astonishing implications. A typical American breakfast supplies an enormous amount sugar and starches which are very quickly converted to blood sugar (as much or more as in the Glucose Tolerance Test), which drives the blood sugar so high as to increase calcium within the cells. Many Americans eat this much sugar at two or even three meals per day.
The resulting high calcium level in the insulin-producing cells of the pancreas makes them over-react and release too much insulin (Resnick 1993), which causes the blood sugar overshoot known as hypoglycemia. Ordinarily, the glucagon-producing cells of the pancreas would kick in, making glucagon to tell the liver to get some of the blood sugar stored as glycogen, but high insulin levels inhibit glucagon production. So the blood sugar continues to fall until the body declares an emergency and calls for adrenalin to raise it. Voilà, we have adrenalin-caused hypoglycemic symptoms of nervousness, irritability and the like.
But wait, there's more!
Dr Resnick's "Ionic Hypothesis" holds that high calcium makes the cells of blood vessel walls constrict more readily, causing higher blood pressure. It makes muscle and fat cells less responsive to insulin, so more insulin is necessary to maintain normal blood sugar. But hyperinsulinemia is associated with weight gain, and, with high blood pressure, with heart disease. Eventually, blood sugar regulation may need more insulin than the pancreas can make so non-insulin dependent diabetes results (Resnick 1993).
In rats, permanent high insulin levels developed after a time proportional to the amount of sugar in their diets. Although their insulin levels normalized when sugar was withdrawn, the hyperinsulinemea reappeared in days when sugar was reintroduced, so the damage is permanent (Yudkin 1972). Significantly, sugar in the diet of rats reduced their life span (Dalderup 1969). In humans, non-insulin dependent diabetes can be controlled by diet and exercise, but control is lost if the diabetics return to their old ways. Sugar in the diet causes permanent injury to the calcium channels of the cells.
Why is this hypothesis compelling? Because calcium channel blockers such as magnesium and Dilantin both decrease blood pressure and lessen hypoglycemia (Sanke 1986). Is hypoglycemia a stage in the development of the overweight, hypertension, diabetes (see graph below) and heart disease responsible for half of all American deaths each year?
Recall that researchers lost interest in relative hypoglycemia because the symptoms had no apparent cause. High calcium in the brain and nervous system resulting from high blood sugar causes "potentiated neurotransmitter release and increased sympathetic nerve activity" (Resnick 1993). This means that wandering blood sugar has an effect on how much of which neurotransmitters (including the endorphins) are secreted in the brain! Since some neurotransmitters in the brain are excitatory and others inhibitory, this will certainly change our consciousness, but in some unpredictable way. However, "increased sympathetic nerve activity" means we are likely to feel more nervous.
So there is now an explanation for the symptoms of relative hypoglycemia, the orphan diagnosis discounted by orthodox medicine, and, indeed, by most everybody. I believe it plays a considerable part in the ubiquitous nervousness and irritability of Americans, which appears to be increasing with sugar consumption. Everything I've read suggests to me that the surge in road rage, drive-by shootings, murderous schoolchildren and so forth is linked to our increasing sugar consumption.
When my blood sugar is above normal, I feel slightly irritable and mentally dulled. I thought this was an idiosyncracy of mine until I read that a psychiatrist noticed a "dementia" in diabetics with high blood sugar. Her diabetologist husband started testing his new diabetic patients for short-term memory defects and found "half my new patients indeed display this mild form of dementia, which appears to lift after several weeks of improved blood sugar control" (Bernstein 1997).
Before I found that a low-carbohydrate,
high-protein diet afforded me close control of my blood sugar, I would cycle
between high and low blood sugar several times a day, so I realize in
retrospect that I had only short interludes of clarity. From my new, more
stable platform of consciousness, I can see others' fluctuations in mood more
clearly. Addressing my own hypoglycemia allowed me to recognize it in my
patients.
§
The fact that hypoglycemia is caused by eating sugar has generally been discounted. This, I'm sure, has much to do with the awesome economic clout of the sugar industry. The price of 150 pounds of sugars for 248 million Americans at 30¢ per pound is about 10 billion dollars. To paraphrase the old joke: Where does a 10 billion pound gorilla sit? Answer: Anywhere he wants to! This particular gorilla has been funding nutrition departments in Universities, educating the people that the Government asks about nutrition in the "harmlessness" of sugar, apparently to great effect. The American Society for Clinical Nutrition, a cradle of orthodoxy, currently acknowledges Coca-Cola, Gerber, Kellogg, Kraft, Nabisco, Nestlé/Carnation and The Sugar Association as "Sustaining Associate Members." In the past, the list has included General Foods, General Mills, Pillsbury and Ralston-Purina. The Government report "Evaluation of Health Aspects of Sugars Contained in Carbohydrate Sweeteners" concluded that "there's no conclusive experimental evidence" that sugar does any harm, other than to our teeth!
This is an outrageous piece of nonsense when you consider that "there's no conclusive experimental evidence" for some 60% of medical procedures, but there's an absolutely staggering quantity of experimental, epidemiological and anecdotal evidence against sugar. However, the Report's conclusion falls upon ears which are all too pleased accept it uncritically - but this is very much akin to telling an alcoholic that red wine protects the heart. There's no doubt in my mind that if sugar were to be introduced as a new product today, the Food and Drug Administration would prevent its introduction into the marketplace.
§
In reading the old studies on hypoglycemia in the medical archives, I learned, among other things, that hypoglycemia worsens allergies, probably causes migraine headaches, and is often associated with rheumatoid arthritis. The story is extraordinary, and worth recounting.
In the early 20's, Dr Seale Harris noticed symptoms in people which were familiar to him from his diabetic patients who had taken too much of the new drug insulin, which had been available for three years. Reasoning that "it seems probable that one of the causes of [hypoglycemia in those who do not take insulin] is the excessive ingestion of glucose-forming foods ...", he prescribed a low-carbohydrate diet with "food of some kind every three hours" which relieved the symptoms of "weakness, nervousness and hunger between meals" (Harris 1924).
Harris and later investigators largely failed
to grasp that "glucose-forming foods" fall into two groups - refined
and unrefined - which have wildly different effects, as we have seen. For
example, an editorial criticizing low-carbohydrate weight-reduction
diets pointed out that "a majority of human beings, particularly
those in
Surprisingly, despite Harris's seminal observation, things remained difficult for hypoglycemics, who had considerable discomfort but no recognizable medical condition which could be treated. Dr Stephen Gyland's experience is interesting in that he himself was a hypoglycemic who later specialized in treating the disease.
"During three years of severe illness I was examined by 14 specialists and 3 nationally known clinics before a diagnosis [of hypoglycemia] was made by means of a six hour Glucose Tolerance Test, previous diagnoses having been brain tumor, diabetes, and cerebral arteriosclerosis ... I found the answer in Dr Seale Harris's diet and immediately recovered" (Gyland 1953). That hypoglycemia was discounted even in those days is revealed by Dr Walter Alvarez' observation that in some thirty years of practice, he had never seen a case of functional hyperinsulinism. Alvarez was a forward-looking physician who practiced at the Mayo Clinic, which Gyland visited in his search for an answer to his problems.
Dr Gyland went on
to practice in
Extraordinarily, although he presented this research before the American Medical Association meeting in 1957, it was ultimately published in an obscure Brazilian medical journal in Portuguese. As early as 1957, the fix was in! Although similar to other compilations of the time, his is unique in its scope and meticulous history-taking. He found well-defined symptom clusters in 49 categories, which I have condensed:
|
Mood symptoms: |
Physical symptoms: |
|
Nervous 94% |
Exhaustion 87% |
|
Irritation, outbursts 89% |
Headache, migraine 72% |
|
Depression 77% |
Digestive upset, ulcer 69% |
|
Insomnia 62% |
Allergies, asthma 43% |
|
Phobias 23% |
Rheumatoid arthritis 24% |
Nervous here means "excitable, easily
agitated, timid", and these symptoms improved with treatment of
hypoglycemia
The prior diagnoses and sources
of refined carbohydrates are intriguing:
|
Previous diagnoses: |
Source of Refined Carbohydrates: |
|
Neurotic 78% |
Sugar, candies, juices 89% |
|
Hypochondriac 76% |
Cereals, bread, pasta, etc 86% |
|
Alcoholic 20% |
Colas, sweetened drinks 84% |
|
Post-partum disorders 19% |
Toast & coffee breakfast 27% |
|
Menopausal 16% |
No breakfast 15% |
The coexisting conditions
fascinated me. Many of Gyland's hypoglycemics
suffered from migraine, and their headaches resolved with treatment of their hypoglycemia.
A study of 421 migraine sufferers found that this is not a coincidence.
"The fundamental metabolic disturbance that usually triggers such
headaches is recurrent hypoglycemia ... [it is suggested that] the term
migraine be replaced by ... 'hypoglycemic headache.'" About 10% of all
Americans have migraine headaches (Roberts 1967).
One in five had been diagnosed as alcoholic.
Recall that alcohol deepens hypoglycemia by distracting the liver from its task
of raising the blood sugar. About 8% of all Americans are problem drinkers
(AHRW 1994).
Three out of four patients - 77% - reported
depression, a very high figure given that, in any given year, only about 10% of
people are treated for depression (Ustüin 1995).
Allergies (such as asthma) and autoimmune
conditions (especially rheumatoid arthritis) frequently coexisted with
hypoglycemia, and resolved when Gyland treated the hypoglycemica. There is a corollary to his observation. The
diabetologist Elliot Joslin
noted that diabetics with high blood sugars rarely suffer from
allergies, peptic ulcer or rheumatoid arthritis. Apparently, both autoimmunity
and allergic reactions are worsened by low blood sugar, while high blood sugar
is protective. About 16% of Americans have allergies, and 13% have arthritis
(
Research has disclosed that anaphylactic
shock (an allergic reaction of life-threatening severity), cannot easily be
induced in animals with normal blood sugar, but occurs readily in animals whose
blood sugars were made low. Further, animals with normal blood sugar were less
susceptible to the common cold (Adamkiewicz 1963). It
has long been known that even the sugar in a glass of orange juice reduces the
effectiveness of the immune system for several hours. Clearly, immune
system activity is modulated by blood sugar level.
I think that people who suffer from these
conditions are very often also suffering from hypoglycemia, which magnifies
their distress to the point where they seek help. But the definition of
hypoglycemia has grown so narrow that many who really are hypoglycemic are told
they are not, according to a strict interpretation of the Glucose Tolerance
Test. The real tragedy here is that these people would derive enormous
benefit from a low-refined carbohydrate diet. However, without the
diagnosis of hypoglycemia, such a diet is not prescribed.
§
Do you or your patients have hypoglycemia?
The first question is: Is the diet
"peculiar?" In other words, does sugar constitute more than 12% of
the carbohydrates in the diet? This is really a trick question because the 150
pounds of sugars in the average diet actually constitutes 45% of the
carbohydrates in the diet: the average diet is itself peculiar! So I ask what
the person has eaten at his or her last three meals. If the answers raise questions
in my mind, I ask:
§ Do you crave any carbohydrate food, and do
you indulge this craving often?
§ Do you take sugar in coffee or tea?
§ Drink sodas most days?
§ Drink fruit juice most days?
§ Eat tropical fruits like bananas, mangos or
dates most days?
§ Eat candy most days?
§ Eat sweet desserts most days?
§ Eat donuts, sweet rolls or cookies most
days?
§ Do you skip breakfast?
§ Do you eat cereal, toast, pancakes and/or
juice for breakfast?
I've found that the more "yes"
answers, the more likely it is that hypoglycemia may be a factor. Then I want
to know about alcohol and caffeine (particularly since caffeine from coffee
turned out to be the cause of Dr Gyland's
hypoglycemia):
§ Do you drink alcohol most days?
§ Do you drink more than two cups of coffee
or tea a day?
§ Do you drink more than two sodas (including
diet sodas) a day?
§ Do you eat chocolate daily?
Again, the more affirmative answers, the
higher my index of suspicion.
Then there are the presenting symptoms.
Consider that hypoglycemia magnifies the immune response, so it often coexists
with allergies (especially asthma) and rheumatoid arthritis. Migraine is a
strong clue. Anxiety, irritation, depression, insomnia and tiredness may have
present causes, but all are worsened by hypoglycemia. Sufferers may be
overweight or, more often in my practice, underweight. And, finally, relatives
with migraine, diabetes, or alcoholism are strong predictors.
Any of these conditions give cause to suspect
that the person will respond to an anti-hypoglycemia diet by becoming less
symptomatic and more responsive to therapy. Here are the answers to some of
these queries among the seven patients whose histories are given at the
beginning of this article:
|
|
SF |
DB |
JR |
WC |
VC |
Dr D |
Mrs D |
|
"Peculiar" diet |
tropical fruit, juice |
cereal, bananas |
cookies |
pasta, sugar |
cake, chocolate |
fruit, juice |
coffee, sugar |
|
Mood swings |
yes |
yes |
yes |
yes |
yes |
yes |
yes |
|
Often tired |
yes |
yes |
yes |
yes |
yes |
yes |
yes |
|
Cravings |
fruit |
sugar, coffee |
cookies |
pasta |
chocolate |
fruit |
|
|
Nervous |
yes |
yes |
|
yes |
yes |
yes |
yes |
|
Underweight |
yes |
yes |
|
|
yes |
yes |
yes |
|
Diabetic blood relatives |
Fa hypo-glycemic |
Mother |
yes |
Father |
|
Grand-mother |
|
|
Alcoholic blood relatives |
|
Father |
AA |
Father |
|
|
Mother |
|
Overweight |
|
|
yes |
yes |
|
|
|
|
Tooth decay |
|
|
yes |
yes |
|
|
|
|
Insomnia |
|
yes |
yes |
|
|
|
|
|
Migraine |
yes |
|
|
|
yes |
|
|
|
Allergies |
yes |
|
|
|
|
|
|
|
Tummy trouble, colitis IBS ulcer |
yes |
|
|
|
|
|
|
Mood swings, tiredness, nervousness and
cravings were the strongest indicators of hypoglycemia in this group.
However, the hard part begins with the suspicion
of hypoglycemia. Most people have considerable resistance to dietary change
unless their health is failing dramatically because disturbances of appetite
are driven by strong, early feelings.
In a perfect world, this would be the moment to
refer the patient for a Glucose Tolerance Test. However, given that
nutritionally-oriented physicians who accept hypoglycemia are thin on the
ground, there are books which can both save counseling time and allow one to
avoid the unpopularity accorded to bearers of bad tidings.
I suggest Dr Atkins' New Diet Revolution
(
For lean people, I recommend Sugar
Busters! (Leighton Steward et al, Ballantine
1998), with the proviso that the authors do not appreciate that fruit juice in
excess can cause hypoglycemia. It's a simple and clear, and quick to read.
I have found that protein at breakfast really
helps. About half the calories from protein slowly become available as
blood glucose, stabilizing the blood sugar for hours (Conn
1936, Thorn 1944). Importantly, an appetite for breakfast quickly reappears
when refined carbohydrates are avoided. Snacks help if meals are more than
a few hours apart. Dr Atkins' brand of low-carbohydrate bars work well.
After a week or so, all my
hypoglycemic patients had to be steered away from some explosively glycemic food such as Grape Nuts, rice cakes, café latte,
rolled oats or soy milk which they mistakenly perceived as wholesome. It helps
to think "carbohydrate addiction" because this process is akin to
counseling substance abusers.
If symptoms persist and a second history
doesn't reveal poor compliance, I refer the patient to a physician for a
Glucose Tolerance Test. Some physicians encourage patients to buy a blood sugar
meter such as the
1 This is familiar to insulin-dependent
diabetics as a "Somogyi reaction", in which
the adrenalin can drive the blood sugar to high levels after it falls below
normal in an "insulin reaction."
4 The American Society for Clinical
Nutrition, a cradle of orthodoxy, currently acknowledges Coca-Cola, Gerber,
Kellogg, included General Foods, General Mills, Pillsbury and Ralston-Purina.
§
Physicians do not suspect hypoglycemia, and psychotherapists
are not trained to recognize it. However, extrapolating from the number of
patients in my practice who responded positively to dietary changes with
improvements in both psychological functioning and physical symptoms, it seems
likely that a great many Americans suffer from hypoglycemia. A few questions
about the seemingly trivial matter of diet can effect a dramatic improvement in
the quality of life.
... back to Contents or on to Sugar ...
AHRW, Alcohol Health and Research World,
1994;18(3):243-5
Adamkiewicz, VW, A New View of the Old Cold - as Sugars go up,
Hypersensitivity Drops, JAMA,
Anderson JW et al; Effects of Carbohydrate
Restriction on Glucose Tolerance of Normal Men and Reactive Hypoglycemic
Patients, Am J Clin Nutr,
1975;28:748-755
Anthony, Dick et al; Personality Disorder and
Reactive Hypoglycemia, A Quantitative Study, Diabetes,
1973;22(9):664-674
Barbagallo M and Resnick LM; The role
of glucose in diabetic hypertension: effects on intracellular cation metabolism, Am J Med Sci, February 1994;307 Suppl
1:S60-S65
Bernstein, Richard, Meaningful Screening Test
for Reactive Hypoglycemia, Diabetes Care, 1987;10(6):792-3
Blass, E et al; Milk-induced analgesia and
comforting in 10-day-old rats: opioid mediation, Pharmacol Biochem Behav, January 1988;29(1):9-13
Blass E et al; Pain-reducing properties of
sucrose in human newborns. Chem Senses,
February 1995;20(1):29-35
Blass, E et al, Interactions between sucrose,
pain and isolation distress, Pharmacol Biochem Behav, March
1987;26(3):483-489
Charles MA et al: Comparison of Oral Glucose
Tolerance Tests and Mixed meals in Patients with ... Hypoglycemia, Diabetes
June 1961;30:465-470
Crapo, P et al, Postprandial Plasma-glucose
and -insulin Response to Different Complex Carbohydrates, Diabetes,
1977;26(12):1178-1183
Dalderup, LM et al; Influence of Extra Sucrose in the Daily
Food on the Life-span of Wistar Albino Rats, Nature,
1967;222:1050
Fabrikant, M; The Problem of Functional Hypoglycemia Attributed
to Nervous Causes, Metabolism, November 1955;IV(6):469-479
Fariss, BL; Prevalence of Post-glucose-Load Glycosuria and Hypoglycemia in a Group of Healthy Young
Men, Diabetes, 1974;23:189-91
Ford, C et al; A psychiatric study of
patients referred with a diagnosis of hypoglycemia, Am J Psychiatry,
1976;133(3):290-294
Fullerton D et al; Sugar, opioids
and binge eating, Brain Res Bull, June
1985;14(6):673-680
Gyland, S; Functional Hyperinsulinism
in General Practice, JAMA, 1957;163:1507
Gyland, S; Possibly Neurogenic
Hypoglycemia, JAMA,
Harris, Seale; Hyperinsulinism
and Dysinsulinism, JAMA, September
1924;83(10):729-737
Harris, Seale; Neurologic
Hyperinsulinism, Southern Medical Journal,
1935;28(11):959-965
Harris, Seale; The Diagnosis and Treatment of
Hyperinsulinism, Annals of Internal Medicine,
1936;10:514-33
Hawkins, R and Pauling,
L; Orthomolecular Psychiatry, Freeman 1973; p 222, 454
Hoffman, RH and Abrahamson, EM; Hypersinulinism - A Factor in the Neuroses, American
Journal of Digestive Diseases, 1949;16(7):242-247
Himwich, H; A Review of Hypoglycemia, It's Physiology and
Pathology, Symptomatology and Treatment, Journal
of Digestive Diseases, January 1944;11(1):1-8
Hofeldt, FD; Reactive Hypoglycemia, Endocrin.
& Metab. Clin's of
JAMA (Journal of the American Medical Association) editorial; A Critique of
Low-Carbohydrate Ketogenic Weight Reduction Regimens,
1973;224(10):1415-1418
JAMA (Journal of the American Medical Association) editorial; Postinfusion Hypoglycemia, 1956;160(10):876
Lesser, M; Blood Sugar and Neurosis,
Nutrition and Mental Health, Hearing before the 95th Congress Select
Committee on Nutrition and Human Needs (1980 Update), Parker House, 1980, page
198
Moersch, FP and Kernohan, JW;
Hypoglycemia, Neurologic and Neuropathologic
Studies, Archives of Neurology and Surgery, 1938;39:242-257
Philips, K; Clinical Studies on the Hypoglycemic
Syndrome, AP-DT, June 1959;10(6):971-977
Price, Weston; Nutrition and Physical
Degeneration, Price-Pottenger Nutrition
Foundation,
Resnick LM; Ionic basis of hypertension, insulin resistance,
vascular disease, and related disorders. The mechanism of "syndrome
X". Am J Hypertens,
April 1993;6(4):123S-134S
Roane DS et al; Continuous sucrose feeding
decreases pain threshold and increases morphine potency, Pharmacol
Biochem Behav
January1990;35(1):225-229
Roberts, HJ; Migraine and Related Vascular
Headaches Due to Diabetogenic Hyperinsulinism,
Headache, July1967, pp. 41-62
Salzer, HM; Relative Hypoglycemia as a Cause of Neuropsychiatric Illness, JAMA, January
1966;58(1):12-17
Sanders, LR et al; Refined Carbohydrate as a
Contributing Factor in Reactive Hypoglycemia, Southern Medical Journal,
1982;75(9):1072-1075
Sanke, T et al; Effect of Calcium Antagonists on Reactive
Hypoglycemia Associated with Hyperinsulinemia, Metabolism,
1986;35(10):924-927
Schoenthaler S; Diet and Crime, Int
J Biosocial Research, 1983;4:25-39
Schoenthaler S et al; The Impact of a Low Food Additive and
Sucrose Diet on Academic Performance in 803 New York City Public Schools, Int J Biosocial Res,
1986;8(2):185-195
Seltzer, HS et al; Spontaneous Hypoglycemia
as an Early manifestation of Diabetes Mellitus, Diabetes,
1956;5(6):437-442
Steinman, R; Biologic Activity in the Tooth
in Health and Disease, The Compendium of Continuing Education,
1984;V(9):722-728
Thorn GW et al; A Comparison of the Metabolic
Effects of Isocaloric Meals of Varying Composition,
with Special Reference to the Prevention of Postprandial Hypoglycemic Symptoms,
Annals of Internal Medicine, 1943;18(6):913-919
USDA Composition of Foods: Vegetables and
Vegetable Products, US Government Printing Office, 1984
USDA Statistical Abstract of the
Ustüin and Sartorius, Mental
Illness in General Health Care, World Health Organization, 1995
Virkkunin, M; Reactive Hypoglycemic Tendency among Arsonists, Acta Psychiatr Scand,
1984;69:445-452
Virkkunin, M; Reactive Hypoglycemic Tendency among Habitually
Violent Offenders, Neuropsychobiology,
1982;8:35-40
West, KM; Diet Therapy of Diabetes: An
Analysis of Failure, Annals of Internal Medicine, 1973;79:425-434
Yudkin, John; Pure, White and Deadly, Davis-Poynter, 1972