Vitamin C
Test-tube experiments in which vitamin C metabolites damaged
DNA were recently reported, and another report involved thickening of the wall
of the carotid artery in people taking supplemental vitamin C.
A lie gets half way around the world before the truth
has a chance to get its pants on.
Winston Churchill
These findings are absurd,
but they were widely reported. However,
we do not hear about them when they are refuted. A 1995 Hoffman LaRoche
review which pronounced vitamin C safe
included several studies in which up to 10
grams were taken each day for 3 years.
The review concluded: “higher than RDA intakes of vitamin C have been
associated with several indices of lowered
cardiovascular disease risk including increases in HDL, and decreases in LDL
oxidation, blood pressure and cardiovascular mortality.”
However, a 2004 study of the Third National Health and
Nutrition Survey data found that vitamin C depletion
and rank deficiency are actually widespread, affecting one person in 3:
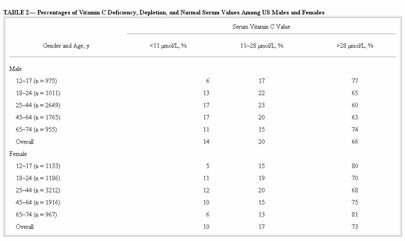
This is incredible.
The table shows that, for example, 17% of males aged 25 to 44 have a
blood level less than 11μmol/L, which
means that they are deficient in vitamin C and are in danger of developing
scurvy. Scurvy! Now this is news –
but who’s ever heard of it?
No wonder an analysis of the First National Health and
Nutrition Survey data found a 42% and a 25% reduced
risk of death for men and women respectively who got the most vitamin C
from diet and supplements compared with those who got the least. A recent meta-analysis of 9 such studies
found that those who took more then 700 mg of vitamin C per day were 25% less
likely to develop CVD than those who got less.
Maybe someone should alert the American Heart Association.
Meanwhile, let us ponder what makes vitamin C so effective in
the prevention of CVD. One of vitamin
C’s most important functions is in the production of collagen, and this is the
function that fails in scurvy, and is compromised in “vitamin C
depletion.” The following section is
technical, but the premise is simple: if vitamin C is in short supply, then
collagen formed for repair of the arterial wall will be weak and vulnerable to
oxidized cholesterol, mechanical stresses, homocysteine and other noxious
influences in the bloodstream. Some have
suggested that this is the fundamental cause of heart disease, and propose a
simple strategy for relief. This
strategy has been patented, experimentally tested and found to be effective,
and is commercially available.
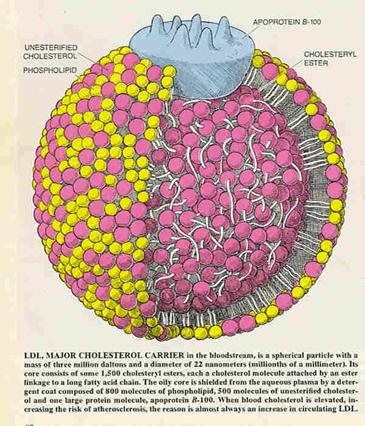
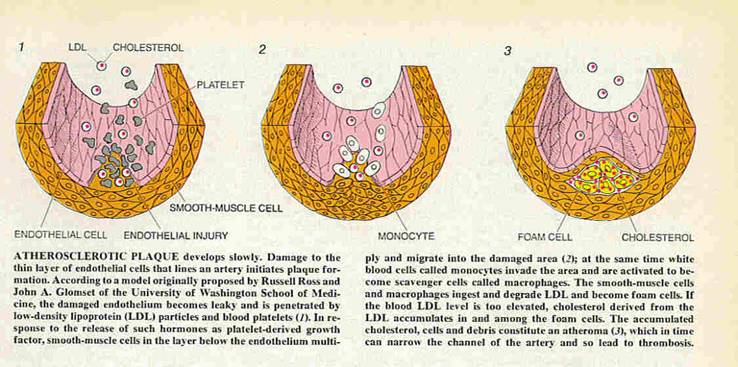
The illustration is from Michael Brown and Joseph Goldstein’s
article “How LDL Receptors influence Cholesterol and Atherosclerosis” in the Scientific American magazine of
November, 1984:
Brown and Goldstein
received Nobel Prizes for elucidating the structure of the LDL cholesterol
receptor, which is how cells get supplies of the cholesterol they need. Their premise that: “Damage to the thin layer
of epithelial cells that lines an
artery initiates plaque formation” is generally accepted. The epithelial cells line the intima, the
inner wall of the artery, sealing the supporting middle of the wall away from
the blood, and actively secreting substances such as prostacyclin and nitric
oxide which modulate both the slipperiness of the blood and its tendency to
clot, and the muscular tension in the wall of the artery which in turn
regulates blood pressure.
How does the epithelial layer sustain damage? From homocysteine, a toxic amino acid which
builds up in the blood if vitamin B6, folic acid or vitamin B12 are in short
supply. By mechanical injury from the
turbulence of the blood flow, or from the contraction of the heart muscle in
the case of the coronary arteries. Or by
infections with bacteria such as Chlamydia pneumoniae
which was found in 55% of atherosclerotic plaques in this study (Emerging Infectious
Diseases 1998, 4(4))
which raises C-Reactive Protein levels, a risk factor for heart disease. Or infection by nanobacteria,
ubiquitous tiny organisms which form calcium overcoats, and which may be the
cause of hardening of the arteries, and kidney stones and prostatitis
besides. Calcium salts do cause
inflammation (Circ Res 2005; 96:1248), and can be removed by chelation; and when chelating agents
are given with tetracycline which kills the nanobacteria, there may be relief
from heart symptoms such as angina. Or
from oxidized cholesterol, caused by either insufficient antioxidants in the
circulation, or acquired from food cooked in over-used cooking fat.
Or the damage may be caused by
poorly-formed collagen which is not strong enough to support the endothelial
cells. In this scenario, the epithelium is torn open
as the poorly-formed collagen beneath breaks apart. This would explain why plaque is found at
points of mechanical stress from turbulence in the bloodstream such as in the
aorta and at bifurcations of the arteries, and from the mechanical stresses
which flatten the coronary arteries with each heartbeat.
Collagen and mucin together form the ground substance which exists between the cells. Just as concrete reinforced with steel is tougher than its components, so do collagen and mucin together form the tough, composite “glue” which literally holds us together. Mucin binds water which gives a shock-absorbing texture to the ground substance, which is in a constant state of flux as it is degraded by enzymes and replaced with newly-synthesized material in the normal course of metabolism. Mucin is an old name for what are now called mucopolysccharides, or the glycosaminoglycans – for simplicity, let’s stick with mucin!
The collagens are the most common proteins in the body. They are found in the skin, in the bones
(which are mineralized collagen), teeth, gums, tendons and ligaments, and give
strength and elasticity to the blood vessel walls. Even the plasma of the blood is a form of
collagen.
This stuff may be more familiar as glue, Jello and
gelatin. When animal skins and bones are
rendered into glue, the collagen they contain is hydrolysed (meaning water is
added) so that it becomes more liquid.
Then, as the glue dries, the water is removed and the cross links
re-form (cross links are the links between the strands of collagen). With less rendering, the mucin survives and
binds water to give Jello, or, if the water is removed, gelatin.
The presence of vitamin C triggers the synthesis of collagen
in a dose-dependent fashion, meaning the more vitamin C, the more collagen is
made. The process starts with mRNA
copying the DNA template for the protein, forming pro-collagen. Then the pro-collagen is hydroxylated, which means the reaction in which an hydroxyl radical
(-OH ) replaces hydrogen (-H ) in the synthesis of a molecule. Each hydroxylation reaction uses up one
molecule of vitamin C. Here is an
illustration of the process from a textbook of biochemistry:
We start inside the part of the cell devoted to protein
synthesis, the rough endoplasmic
reticulum. Here, pro-collagen is made from the RNA
template and then hydroxlylated,
which means -OH’s are added, and each -OH added consumes one molecule of
vitamin C (unlike in vitamin C’s antioxidant function, where it is
reversibly oxidized and lives to fight another day, hydroxylation
irrevocably consumes the molecule).
The pro-collagen passes through a pore called a ribosome into the cytoplasm of the cell (the many ribosomes on the surface of the endoplasmic reticulum
give it a rough appearance, hence “rough endoplasmic reticulum”) where it
is elaborated with sugars, and then it passes out of the cell into the
intracellular space. Here, vitamin
B6 acts as a co-enzyme for the copper-dependent enzyme lysyl oxidase which cross-links the pro-collagen strands to
form collagen (Bird, TA et al, Lysyl oxidase: evidence that pyridoxal
phosphate is a cofactor. Biochem Biophys Res Comm 1982; 108(3):1172-80). Further, the active form of B6, pyridoxal
phosphate, has been found to be low in atherosclerosis. (Serfontain W et al, Plasma P5P level as risk index for
coronary artery disease. Atherosclerosis 1985; 55:357-61). Weight
for weight, strands of collagen are stronger than steel. As elastin,
collagen gives the blood vessels the elastic resilience they need to cope
with the pressure pulses of the heartbeat.
Anything that interferes with collagen synthesis or repair – such as
a shortage of vitamin B6 – will cause the arteries to deteriorate. (Levene CI et al, The aetiological role of maternal B6
deficiency in the development of atherosclerosis. Lancet 3/19/77; 1(8012):628-30
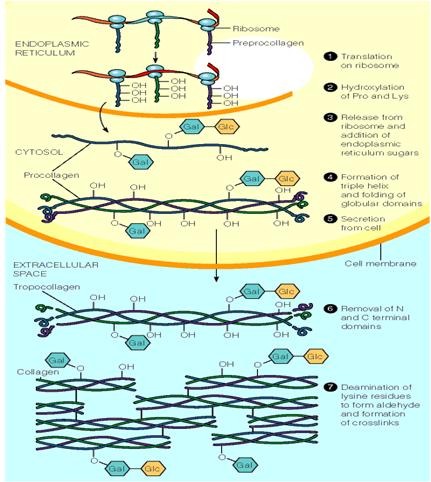
Hydoxylation takes place in step number 2, and each -OH costs
one molecule
of vitamin C. If vitamin C is in short
supply, fewer –OH’s will be attached to the pro-collagen so that the cross-linking
of the collagen fibers in step number 7 will be incomplete, and the collagen
cannot attain its full strength.
Other deficiencies which affect this process include vitamin
B6 deficiency which weakens the collagen because B6 is the co-factor for lysyl
oxidase, which forms the cross-links in step number 7. One of the symptoms of B6 deficiency is
edema, meaning that with too little collagen, mucin binds more water (like
Jello). Low vitamin B6 therefore means
fewer cross-links and weaker collagen. Too
little thyroid hormone suppresses collagen synthesis and promotes mucin
production in the arterial wall, weakening the composite material and causing
an edema which is called myxedema in the severe deficiency state. The important thing here is that there are
way more heart attacks in those who are low in vitamin C, vitamin B6, and
thyroid hormone.
In scurvy, so little vitamin C is available that collagen
synthesis fails and the circulatory system falls apart, so that half the
victims die of internal bleeding. The
other half die of infections, which underlines the importance of vitamin C in
immune function. One of the most
pernicious errors of assumption ever made is that enough vitamin C to avoid
scurvy is enough vitamin C to maintain health.
The RDA supplies enough vitamin C for some hydroxylation so that the
collagen doesn’t fall apart, but not enough for the collagen to attain its full
strength.
There is clear evidence of weak collagen in the widespread
distribution of wrinkles, stretch marks, poor wound healing, gum disease,
chronic back pain, high cholesterol, gallstones and
cataracts, atherosclerosis and tooth decay.
Another requirement for vitamin C is in the production of
bile. As with the synthesis of collagen,
a molecule of vitamin C is used up in the hydroxylation of each molecule of
cholesterol elaborated to form bile, which is essential for emulsifying fats
during digestion. It follows that if
vitamin C is in short supply we can’t excrete so much cholesterol, so we tend
to develop gallstones
and an elevated cholesterol level as a consequence. A second reason that cholesterol rises if vitamin
C is in short supply is that vitamin C itself inhibits the enzyme HMG-Coenzyme A
which is responsible for the production of cholesterol:
Since inhibition of HMG-CoA reductase occurs at physiological concentrations of ascorbic acid in the human leukocyte (0.2-1.72 mM), this vitamin may be important in the regulation of endogenous cholesterol synthesis in man.
Statin drugs are synthetic HMG CoenzymeA
inhibitors, but vitamin C is a natural
HMG CoenzymeA inhibitor, which is entirely without
side-effects. Thus, a vitamin C deficiency raises the cholesterol level in the blood,
and high-dose vitamin C supplementation lowers cholesterol levels in those
whose levels are elevated (Gaby SK et al, eds, Vitamin Intake and Health:
A Scientific Review. Marcel Dekker NY, 1991).
Vitamin C is concentrated to levels many times that in the blood in the specialized white blood cells of the immune system. Neutrophils actively take up oxidized vitamin C and recycle it into vitamin C once more until the concentration within the cell is 10 times that in the plasma. If bacteria are present, the neutrophil becomes “activated” and concentrates vitamin C a further thirty times. This protects the neutrophil while it uses oxidants to attack the bacteria. Immunity is severely degraded if the white cells cannot get enough vitamin C, and vitamin C is quickly depleted in even minor infections.
But to return to our torn collagen. In 1984, Brown and Goldstein wrote that: “the
damaged endothelium becomes leaky and is penetrated by low-density lipoprotein
(LDL) particles ...” Since then, in
1990, Mathias Rath and colleagues showed that the
form of cholesterol which accumulates in plaque is not LDL, but rather lipoprotein(a),
which consists of LDL attached to apoprotein(a). An apoprotein
is the protein part of a lipoprotein, and a lipoprotein is a compound that
carries fats and cholesterol, in the blood.
|
|
So lipoprotein(a) – Lp(a) – is the
new LDL, the new “bad” cholesterol.
Several studies have demonstrated that high Lp(a)
increases the relative risk of heart trouble
by 1.9 in men and 1.6 in women. Women
who had both high Lp(a) and
C-reactive protein had a whopping 3.67 time the odds of developing
CHD. In a 1997 study,
the mean level of Lp(a) for those with clean coronary
arteries was 115 mmol/L, while those who had blockages in all three coronary
arteries had a mean level of 305 mmol/L.
However, perhaps because no drug is available which will lower Lp(a), remarkably little attention has been paid to this
discovery.
|
|
There may be two reasons for the atherogenicity of Lp(a). First, it is
similar enough to plasminogen that it inhibits the dissolving of clots. Second, it sticks to lysine and proline, the amino acids exposed when poorly-formed
collagen tears open.
Linus Pauling’s
take on this was that if we have enough vitamin C, collagen is made with it to
repair damage to the arterial wall. If
we don’t, we use lipoprotein(a) to repair the tear as it binds the exposed
lysyl residues of the damaged collagen together, which is to say that Lp(a) is a surrogate
for the missing vitamin C. But if the
low-C state of affairs continues, plaque forms and thickens as white cells
infiltrate the damaged area and the smooth muscle cells of the arterial wall
proliferate, there is calcium infiltration (the -sclerosis part of
atherosclerosis), and eventually the plaque ruptures and there is a heart
attack.
Interestingly, plaque is found in every human population
studied the world over. Even some of the
young men in Barcelona,
where the rate of heart attack is very low, have plaque. Amazingly, plaque is as prevalent in Japanese people, although their rate of heart
attack is one sixth that of
A man is as old as his arteries
But neither atheroma nor Lp(a) are found in
creatures which make their own vitamin C. Man, the
primates and a few other creatures such as the guinea pig are among the few
creatures on the face of the Earth who do not make vitamin C from glucose in
their livers. Only these creatures
suffer plaque if they cannot obtain sufficient vitamin C, and only man among
these suffers heart attacks. Pauling and Rath investigated the
effect of depriving guinea pigs of vitamin C (who, like us, cannot make their
own), and found Lp(a) in the plaque which formed in their
arteries. Furthermore, feeding 40 mg/kg of vitamin C per day prevented plaque
formation, and prevented accumulation of Lp(a) in the
arterial wall. This is equivalent to
about 3 grams per day for the average human.
This study confirms the results of Dr GC Willis of
Pauling and Rath
published their Unified Theory of Human Cardiovascular
Disease in the Journal of Orthomolecular Medicine in 1992. Then Pauling had
the inspiration that since Lp(a) was sticky for
lysine, then lysine itself should protect against cholesterol deposition in the
arterial wall. Lysine is essential amino
acid, so that it is benign in any reasonable quantity. He found that the combination of vitamin C
and lysine did indeed resolve angina pectoris in a human subject. Angina is like a cramp, a pain on exertion
caused by reduced blood flow to the heart muscle because of plaque-narrowed
coronary arteries. This man was taking
aspirin, lovastatin, CoQ10, and 6 grams of vitamin C
per day among other supplements, and had used up all his available leg veins in
by-pass operations. However, in spite of
employing every available medical remedy, his angina was worsening even with
liberal nitroglycerin use:
In this predicament and with his history of restenosis, I suggested that he continue ascorbate and add 5 g of L lysine daily (ca., six times the lysine derived from dietary protein) to try to mitigate the atherosclerotic acitivity of Lp(a). After reading the 1990 Rath and Pauling reports and their manuscript titled "Solution to the puzzle of human cardiovascular disease", he began taking I g of lysine in early May 1991 and reached 5 g (in divided doses eight hours apart) by mid June. In mid July, his HDL was, as usual, a low 28 mg/dl. A low normal 0.9 mg/dl blood creatinine indicated that lysine could be increased, if needed. He could now walk the same two miles and do yard work without angina pain and wrote, "the effect of the lysine borders on the miraculous". By late August, he cut up a tree with a chain saw, and in early September started painting his house. By late September, possibly from over exertion, he again began to have angina symptoms during his walks, but after stopping strenuous work and increasing lysine to 6 g [calculated to provide a peak 280,000 molar excess in the blood over his then 6 mg/dl of Lp(a) to help compensate for the relatively high dissociation constant of lysine Lp(a)] these symptoms stopped entirely by mid October. His blood creatinine was still a normal 1.2 mg/dl. He attributes his newfound wellbeing to the addition of lysine to his other medications and vitamins. His wife and friends comment on his renewed vigor. (Pauling L, Case Report: Lysine/Ascorbate Related Amelioration of Angina Pectoris. J Ortho Med 1991, 6(3-4):144 46)
Pauling patented this treatment for heart disease, in the
first such patent ever granted, and further patented the use of the technique
for cleaning plaque from
organs to be used in transplants.
Linus Pauling
died on
Discovery is seeing what everybody else has seen,
and thinking what nobody else has thought.
Albert Szent-Györgyi
Szent-Györgyi pointed out in his Nobel
Prize acceptance speech that ascorbic acid by itself doesn’t resolve
scurvy:
At the time that I had just
detected the rich vitamin content of the paprika, I was asked by a colleague of
mine for pure vitamin C. This colleague himself suffered from a serious haemorrhagic diathesis [meaning capillary bleeding as is
found in scurvy]. Since I still did not have enough of this crystalline
substance at my disposal then, I sent him paprikas.
My colleague was cured. But later we tried in vain to obtain the same
therapeutic effect with pure vitamin C. the ascorbic acid complex which
includes vitamin P B the bioflavonoids B is necessary to do that.
Incredibly, by 1937, Szent-Gyögyi
had deduced that the vitamin C complex (not just vitamin C) neutralizes the
oxygen free radical (a term not yet invented!) in two stages:
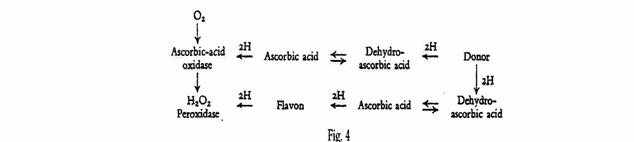
Ascorbic acid oxidase oxidizes [ascorbic] acid with
oxygen to reversible dehydro-ascorbic acid, whereby the oxygen unites with the
two labile H-atoms from the acid to form hydrogen peroxide. This peroxide
reacts with peroxidase and oxidizes a second molecule of ascorbic acid. Both
these molecules of dehydro-ascorbic acid again take up hydrogen from the
foodstuff .
But peroxidase does not oxidize ascorbic acid directly. I
succeeded in showing that another substance is interposed between the two,
which belongs to the large group of yellow, water-soluble Y plant dyes (flavone, flavonol, flavanone). Here the peroxidase oxidizes [the flavon, the bioflavonoid] which then oxidizes the ascorbic
acid directly, taking up both its H-atoms. (ibid)
The significance of this is that a bioflavonoid such as the
hesperidin (found in the white part of the orange rind), rutin,
quercetin and so forth are needed for vitamin C to perform its antioxidant
function, and they modulate the permeability of the capillaries – hence vitamin
P. They are themselves potent antioxidents, and many also display metal binding activity,
a property which may contribute to their antioxidant effects. So what
we think of as vitamin C is actually ascorbic acid, a fraction of the vitamin C
complex. Ascorbic acid does not cure
scurvy, it is the vitamin C complex – ascorbic acid plus bioflavonoids - which
cures scurvy.
Parenthetically, Ancel Keys retired to southern
The Lyon Heart Study was an
intervention trial (first reported in 1993) in France that demonstrated that a
diet resembling the Cretan diet, i.e. rich in plants and alpha-linolenic acid
from canola oil, afforded better protection from the recurrence of myocardial
infarction than the Step I American Heart Association prudent diet.
In the Cretan diet, the
intake of alpha-linolenic acid is high due to the consumption of herbs,
walnuts, seeds, snails, purslane, and lamb. The Lyon Heart Study is important
because it provides the first clinical proof of a protective effect of the
Mediterranean diet on cardiovascular disease.
(Mediterranean
diet)
Many others have noticed this. For example, this is from a website offering
high-ω3 eggs:
Surprisingly, the men from
The Missing Clue
Two decades later, one of the
rinsing clues was provided: the traditional
The result of the study made
medical history. Just four months into the clinical trial, the researchers
discovered there had been significantly fewer deaths in the group on the
modified
At this writing, the American Heart Association still offers
its so-called prudent diet, and suggests ω3 supplements be used only by
those at special risk. It is sobering to
reflect on the numbers of lives lost because Keys ignored his own observation
of the life-saving nature of the diet of
A Trial of Pauling’s
Heart Disease Therapy
Mathias Rath went on to publish a trial of nutritional
supplements including 2.7 grams of vitamin C and 450mg each of lysine and proline in people with heart disease in 1996. He demonstrated that early, small calcified plaques
disappear entirely, and more extensive plaques grow at a decreasing rate. The study duration of one year was apparently
too short for these plaques to cease growing and start shrinking as the early,
small plaques had done, but that was clearly the trend:
The American Heart Association may never acknowledge this
simple effective strategy, but it is available to those in need through Tower Heart Technologies.
Confirmation that vitamin C is effective against
atherosclerosis comes from another source.
Doctor of Optometry Sydney Bush published
in a letter in the July, 2004, British Medical Journal that in the course of
his usual practice of placing patients on vitamin C to prevent or treat contact
lens problems, he had serendipitously discovered that high-dose vitamin C
reversed arterial disease. Using a
digital retinal camera, he saw that small aneurysms, bulging areas that
indicate weak artery walls, in photographs of
the retina resolve with supplementation.
Bush believes that over 90% of patients with arterial disease can be
improved with 3000 milligrams of vitamin C per day, but some need over
10,000mgs/day supplemented with extra vitamin E. Even hard calcifications,
which look like a fine white line that runs down almost every artery of adults
who have high cholesterol, disappeared over a two-year period of vitamin C
supplementation.
Other observations suggest that vitamin C is protective
against both atherosclerosis and heart attacks.
For example, in a population of Finns, serum vitamin C below the
threshold of deficiency elevated heart attack risk by 4 times. The researchers concluded:
To our knowledge, our current
results are the first empirical evidence in humans to show that vitamin C
deficiency, as measured by low plasma ascorbate
concentration, is a risk factor for coronary heart disease. In our cohort
plasma vitamin C concentration above the limit of deficiency was not associated
with the risk of acute myocardial infarction. Thus, high intakes of vitamin C
or vitamin C supplements would probably not reduce the risk of acute myocardial
infarction. Our findings suggest, instead, that if a minimal necessary
requirement of vitamin C is not met the risk of myocardial infarction is
increased. (Nyyssönen K et al, Vitamin C deficiency
and risk of myocardial infarction: prospective population study of men from
eastern
After Linus Pauling
published How to Live Longer and Feel
Better in 1979, vitamin C production
climbed in
Using the Nurses Health Study data, Dr Walter C Willett of Harvard
looked at vitamin C intake and risk of coronary
heart disease in women. He concluded
that vitamin C supplement use was associated with a lower risk of CHD (RR =
0.72; 95% CI 0.61 to 0.86). This means
he found that the women who took supplemental vitamin C were, on average, 28%
less likely to develop heart disease as the women who did not.
This is remarkably consistent with the results of a study of
the Second National Health and Nutrition Survey which found a 21% to 25%
decreased risk for heart death, and 25% to 29% decreased risk of all-cause
mortality in people with normal to high serum vitamin C. The study’s conclusion was that “increasing
the consumption of ascorbic acid ... could decrease the risk of death among
Americans with low ascorbic acid intakes.”
Among women in this population, the blood vitamin C level was associated
with “protective” HDL cholesterol, which increased by 2 mg/dl for each 1 mg/dl
increase in serum ascorbic acid level.
Linus Pauling
said in his last interview:
I don’t know if there’s a need
for a randomized, prospective double-blind study when you get evidence of this
sort about the value of a large intake of vitamin C and also lysine for
preventing the deposition of atherosclerotic plaques and preventing death from
cardiovascular disease. I recommend that
every person, every adult, take 3 grams of vitamin C a day and smaller amounts
for children proportional to body weight.
That every person who is at risk for one reason or another for
cardiovascular disease take perhaps not only 6 grams of vitamin C per day but
also 2 grams or more of lysine a day.
Two grams may well be protective, but larger amounts might be needed for
greater risk of cardiovascular disease.
Clearly, there is a huge difference between the 90mg RDA for
vitamin C and the amount we can profit from.
Consider that intravenous vitamin C in gram quantities cured even polio
in the epidemic of the 1950s when it was administered by Dr Frederick
Klenner. Dr Thomas Levy reviewed the
literature in support of the proposition that vitamin C in sufficient quantity
can cure all known bacterial and viral conditions if administered intravenously
in his book Vitamin
C, Infectious diseases and Toxins (Xlibris,
2002). This implies that we benefit from
larger amounts when we’re sick, and this is confirmed by the fact that most
creatures make their own in great quantities - the equivalent of many grams for
a human - when they’re ill.
But although even steadfast nutritional conservatives
acknowledge that illness depletes us of vitamin C, we don’t learn this from the
author of the RDAs, the National Academy of Sciences, who cap the safe intake
at 2 grams on the grounds that more may cause diarrhea – never mind that in
sickness, Dr Robert Cathcart
has established that this “bowel tolerance”
increases (depending on the severity of the condition) up to hundreds of
grams for life-threatening diseases such as AIDS. Nor do they share that man is the only
creature to suffer from atherosclerosis.
As we have seen, experimentation suggests that supplementing C to mimic
the levels found in creatures that make their own causes atheroma to recede and
perhaps eventually to disappear. It
seems likely that with sufficient vitamin C in the diet, atherosclerosis might
not occur.